Ventilators Alone Won’t Save Us

During an unusually calm shift in the intensive care unit, Barbara (a pseudonym), the experienced doctor on staff, asked me and the resident physicians to sit around the table in the break room. To teach us how to read ventilator curves on a monitor, she instructed us to inhale and exhale following its rhythm. We all breathed in and out, filling and emptying our lungs with air, mimicking the waves of the beeping monitor. This kind of self-reflexive learning about normal and abnormal breathing patterns is how ventilators get incorporated into the everyday work of critical care providers.
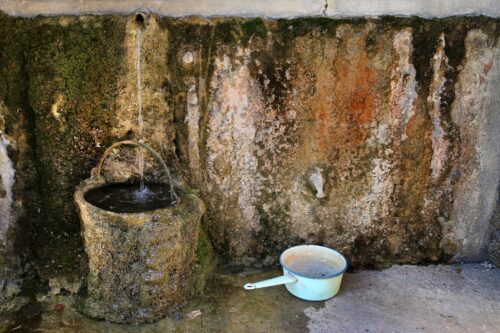
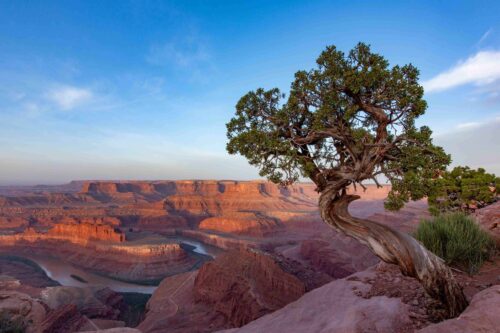
While conducting fieldwork in Buenos Aires, Argentina, in 2018 for my doctorate in medical anthropology, I spent many hours learning about the seemingly simple act of breathing. I witnessed the complex, intimate relationship between ventilator machines, patients, and the doctors tasked with working in critical care. Noticing the contrast between patients struggling on ventilators and my own healthy lungs, I was repeatedly reminded that we often notice the presence of things through their absence.
Because of the severe respiratory symptoms that can be brought on by the novel coronavirus, ventilators have been at the center of the response to the COVID-19 pandemic. Since the outbreak, ventilators have been praised, mystified, politicized, demonized, and everything in between. Fear of ventilator shortages was at the forefront of the response controversy in March. And while health care workers have been hailed as heroes, ventilators have become pawns in political debates and a currency in both national and international relations. Ventilator machines have been shipped from China to Italy, and from California to New York. While the biomedical manufacturing industry ramped up production, auto manufacturers like Ford and GM began making simplified versions of breathing machines.
Now, in mid-May, the U.S. finds itself with a ventilator surplus, and President Donald Trump, the self-proclaimed “king of ventilators,” is even planning on shipping a portion of them to foreign countries in need.
But what has been missing in many of these discussions is an obvious yet fundamental fact: Ventilators do not operate themselves. Even as the production of ventilators catches up with the unprecedented demand around the globe, ventilators still need skilled—and physically and psychologically healthy—staff to operate them properly. One ventilated patient requires at least two health care professionals per shift.
The pandemic has made the already existing shortage of trained ICU personnel become more evident. Medical staffs are working long hours in difficult conditions, they are at an increased risk of infection from the virus, their family lives are disrupted, and they are more vulnerable than ever to burnout. An abundance of ventilators without the staff to operate them—or with staff who are overworked, burned out, or themselves sick with the virus—is no solution at all.
When I sat down with Barbara and the residents in an Argentine ICU in 2018, I never imagined that ventilators would be the protagonists of a global pandemic. Breathing is a vital function. Now we have all been harshly reminded of exactly how critical it is.
In ICUs, the most acute patients are—quite literally—out of breath. These patients are sedated, intubated, and put on a mechanical ventilator that provides additional breathing support. As I witnessed in the wards in Argentina, even while sedated, patients sometimes violently resist intubation and need to be restrained. Finding their airways blocked by a tube in their throat, they often try to pull it out themselves. Then there’s ICU delirium: Some patients report having experienced intense sensory confusion and emotional disruption, including hallucinations, delusions, and paranoia, during sedation.
It’s important to recognize that while ventilators are an integral part of critical care, they are not therapeutic per se, since they do not cure what the patient is suffering from. Ventilating a patient just provides additional breathing support and buys time.
As every intensive care professional knows, putting someone on a ventilator—and weaning them off—is an extremely delicate operation that poses at least as many risks as advantages. For one, ventilated patients have a higher risk of bacterial infection. Furthermore, when done improperly, ventilation can cause acute lung injury. Life after ventilation almost always involves lengthy physical rehabilitation, and some patients experience PTSD-like symptoms in what is called post-intensive-care syndrome. Yet, as I learned during my research in ICUs, often—especially now in the time of COVID-19—ventilation is the necessary last resort.
Putting someone on a ventilator poses at least as many risks as advantages.
Physicians must also take into account details about a patient’s history and make risk assessments under extreme pressure. “When you place someone on a ventilator, you have to take into account various factors: Do they have any previous heart or respiratory conditions? Are they at risk for organ failure?” explains Dr. Luca Bastia, a personal friend and an ICU doctor in Milan, Italy. Physicians must then determine the settings of the ventilator based on patient weight, levels of oxygenation in the blood, and number of breaths per minute.
After these parameters are set, the machine performs the task on the patient by pushing the breathable, oxygenated air down the breathing tube into the lungs. The lungs then fill with air and the chest inflates and deflates as carbon dioxide is let out. The skilled setting of this complex machine—How much oxygen? How much pressure? For how long?—is a fundamental aspect of ICU doctors’ training and daily work. “Adjusting the ventilator settings, depending on how the patient is reacting, is an art,” says Bastia.
As more data come in and clinical experience managing COVID-19 increases, doctors in ICUs are questioning the efficacy of using common ventilation strategies. The virus affects the lungs differently than other, more familiar respiratory conditions like severe bacterial pneumonia, and therefore the timing and settings of mechanical ventilation are being continually rethought. For this reason, as well as the fact that initial data indicates about 24.5 percent of COVID-19 patients who were on ventilators died, the method is increasingly being used with caution. Instead, doctors are finding success with some patients using noninvasive methods such as high-flow nasal “cannulas,” prongs that sit below the nostrils and blow warm, oxygenated air into the nose. Another “low-tech” solution that has held promise is putting patients on their stomachs, a technique called proning, so that the back of the lungs can open, thus aiding breathing.
Prior to the coronavirus pandemic, health care personnel in wealthy countries like the U.S. and the U.K. had seldom faced the dilemma of considering which patients should receive ventilators when there aren’t enough to go around. But in the last few months, in COVID-19 wards from Lombardy, Italy, to New York City, critical care providers have frequently been confronted with such decisions, sometimes resorting to building makeshift ventilators or attaching one ventilator to two patients.
Health care providers have written about the utter injustice of “fair allocation” and shared the deep distress of even being presented with the decision in the first place. Italian ICU doctors confronted these gut-wrenching choices at the height of the country’s outbreak in March and April, eventually having to operate under the guideline to “maximize the benefits for the largest number of people.”
Recently, the Argentine Society of Intensive Care published an open letter from an ICU physician imploring the public to remember those who ventilate: “When talking about ventilators, please talk about those who operate them. And do not ask us health professionals to enact redistributive justice with ventilators.”
“Redistributive justice with ventilators” might appear to be strongly stated. But during my research, I observed how physicians and nurses—amid equipment shortfalls, administrative frustration, and personal stress—confronted many difficult decisions that often go well beyond what clinicians are trained for.
In ICUs all over the world, professionals are already tasked with assessing the best way forward in treating an unknown virus. But now they are also being asked to take on the moral and societal responsibilities of what comes with a shortage of resources. And making those decisions while working under high-stress conditions affects both patients and health care staff themselves—a reality made tragically clear by the recent deaths by suicide of New York City Emergency Department Physician Lorna Breen and of Italian ICU nurse Daniela Trezzi in Lombardy, among others.
Providing child care, testing, and mental health support are just a few of the concrete ways that health care workers could be better supported by state and local governments. Vital breathing machines that push oxygen into sick patients’ lungs cannot function if the staff who operate them are left gasping for air.
While it is undeniable that ventilators remain critical for treating COVID-19 patients and that ventilator innovation is important, it’s increasingly clear that machines alone will not save us—they rarely do.