Can Social Scientists Help Control Epidemics?

On May 24, 2014, a young woman arrived at the Kenema Government Hospital in Sierra Leone, seeking admission. She had miscarried her pregnancy and doctors feared that she might have Ebola, the contagious virus that can cause internal bleeding and killed 3 in 4 people who contracted it.
Though the young woman survived the sickness, her positive Ebola test signaled the emergence of a raging viral epidemic that would tear through Sierra Leone in a matter of months and eventually kill more than 3,500 people in that country alone. Though international first responders and nongovernmental organizations arrived on the scene to help, they soon realized they were in over their heads.
Even before Ebola, people in the area had little faith in the safety and sanitation standards of their community hospitals. And the epidemic control strategies were sometimes at odds with the population’s sacred customs and traditions. In many cases, the fallout of this clash accelerated the virus’ spread.
When first responders arrived, they observed that people were contracting Ebola through hands-on contact with the deceased. To break this transmission chain, public health teams—often hailing from elsewhere—began confiscating bodies as soon as people died. They forbade family members from watching burials or washing the dead per usual customs. Sometimes, out of fear, health employees resorted to hoisting bodies with poles into unmarked graves.
These and other policies triggered a massive outcry, deepened distrust, and increased people’s reluctance to seek treatment for Ebola. The situation grew so untenable that medical first responders turned to their social science colleagues in desperation.
“The first responders got in touch with us [saying], ‘We are really struggling with the cultural issues. Can you help?’” says Annie Wilkinson, an anthropologist at the Institute of Development Studies then working in Britain and Sierra Leone. Along with a diverse group of social scientists, Wilkinson created the Ebola Response Anthropology Platform (ERAP) to help resolve the cultural logjam that had arisen. This platform would later inspire a second with a broader scope, the Social Science in Humanitarian Action Platform (SSHAP), to build social science insights into epidemic and pandemic control measures going forward.
For decades, most epidemic responses have focused on medical and logistical factors: drafting health guidelines to halt disease spread, building well-equipped treatment facilities, and finding efficient ways to distribute vaccines. But West Africa’s campaign against Ebola was a crucible in which those public health priorities started to shift.
Because biomedical interventions designed to stop Ebola transmission were breeding fear and resentment in local communities, networks like ERAP and SSHAP collaborated closely with government and NGO officials managing the epidemic. A new, socially informed approach to epidemic management began to drive response efforts to epidemics the world over, including those led by national agencies, such as the Centers for Disease Control and Prevention in the United States and international groups like the World Health Organization.
With social scientists’ input, first responders from outside came to see established traditions and values not as obstacles but as foundations for effective disease control. This revised outlook is now shaping the way medical teams around the world are tackling the COVID-19 pandemic.
For the people of Sierra Leone, a majority Muslim country, cleaning and dressing the body of the deceased are integral to traditional burial and mourning practices. This kind of close contact put mourners at risk of contracting the Ebola virus during the 2014–2016 epidemic.
Yet out of reverence for their loved ones, many people held fast to their customs—and they justifiably saw the newly mandated burial practices as insulting to their relatives. One young man felt so strongly about honoring his mother through traditional rituals that he illegally cleaned and dressed her body himself, even though she had died of Ebola. He then traveled out alone into the bushlands surrounding his village, waiting to see whether he would develop the telltale symptoms that would signal his own demise.
The crisis around the upending of Sierra Leonean burial practices was just one of the issues that spurred Wilkinson and other social scientists to train a cultural lens on the problem. More than a dozen experts from Britain, Sierra Leone, and the United States joined forces to develop a plan.
The group used an email listserv to host vigorous discussions about challenges facing first responders, including those springing up in the wake of new burial requirements. The newly formed group, ERAP, received funding from the British government and the Wellcome Trust to develop a more socially attuned approach to epidemic control.
Almost right away, officials inundated the fledgling platform with urgent questions. “We found ourselves advising the WHO,” Wilkinson recalls, “who were just completely overwhelmed and didn’t know what to do.”
While fielding these kinds of calls, experts with the platform worked to make connections between researchers who had specialized local knowledge of virus-affected communities. The team also supported local fieldwork, including interviews with residents of Sierra Leonean towns and villages.
Getting on-the-ground research insights to public health officials was central to ERAP’s approach, Wilkinson says. “One of the big things was getting analysis and briefings out rapidly,” she explains. “Rather than waiting to the end [to] publish our research, it was real-time analysis.”
Roland Suluku, a social scientist and infectious disease expert at Njala University in Sierra Leone, helped head up one early rapid response fieldwork team. He, ERAP anthropologist Paul Richards of University College London, and other colleagues visited about 25 villages. They struck up conversations with community members and local leaders about how epidemic control efforts were affecting them. They also gathered insight into responses to past disease outbreaks.
Over and over, people told Suluku’s team that they viewed health responders’ actions as disrespectful to them and their relatives. Their stories suggested people whisked away bodies and failed to report where the remains were located. People were upset that they could not bear witness to their loved ones’ last rites.
Talks with communities demonstrated that although health teams had developed their burial policies with good intentions, these policies actively interfered with efforts to control Ebola’s spread. Suluku returned from his fieldwork well-prepared to have candid conversations with ERAP colleagues. “I told them, ‘The only way you can allow this epidemic to slow down is to allow people to witness the burial,’” he recalls.
Similar complications arose as Ebola spread through the Democratic Republic of the Congo (DRC) in 2018. In the DRC, SSHAP—the new platform ERAP had inspired—worked with UNICEF-affiliated social science teams who were studying community responses to strict new burial regulations. These responses were sometimes so strong that they spiraled into violence, with people assaulting burial teams and pelting them with stones.
Among the researchers documenting the situation was Omar Sibilondire, a social scientist with UNICEF, who spent long hours in places like hair salons and game rooms, where people gathered to exchange ideas. In these conversations, he says, people expressed concern that medical teams composed of strangers were handling the deceased, when tradition requires that only relatives touch the bodies.
Public health teams were also shooing away grieving relatives so they could put the bodies into enclosed bags. When this happened, “the women cried while saying ‘bonakuya mukamata,’ which means ‘they’ve come to take it,’” Sibilondire says. “This was the source of a lot of tension.”
Medical teams composed of strangers were handling the deceased, when tradition requires that only relatives touch the bodies.
From 2014 onward, interviews and direct observations with people affected by the epidemic helped groups such as the WHO develop and update what they called “safe and dignified” burial practices for Ebola-affected communities. The new guidelines aimed to limit transmission while maintaining traditional funeral rites and procedures to the extent possible.
They recommended placing remains in a body bag to prevent viral spread, but they also specified that a faith leader and family witnesses could participate in the burial process. Families could also choose their own gravesites, rather than settling for mass, hastily dug graves.
With social scientists’ encouragement, medical first responders such as the WHO, the Red Cross, and UNICEF have adopted these recommendations, which, Wilkinson explains, helped families feel more respected and included in the process. “Burial is done by people’s loved ones, people that they know,” she says. “There’s rituals associated with the end of life.”
As a result, many communities proved more willing to take steps that prevented Ebola’s spread after victims died. One analysis of Ebola transmission in Liberia, Sierra Leone, and Guinea suggested that the Red Cross’ safe and dignified burial program prevented as many as 10,000 new cases of Ebola.
The burial crisis was just one part of the larger challenge ERAP and SSHAP social scientists faced in reexamining public health efforts that stirred up fear and mistrust. In Sierra Leone, for example, medical first responders built large, antiseptic-looking clinics to treat Ebola. These “Ebola treatment centers” were sometimes far from affected villages, and their interiors were designed with high physical barriers in exam areas, meaning that people couldn’t see where their loved ones were being taken.
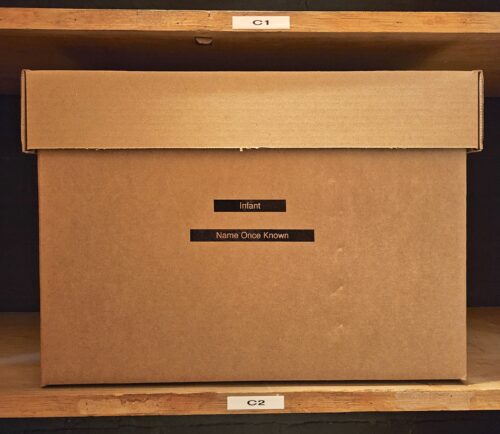
In case after case, families watched health officials whisk their relatives off to unfamiliar facilities from which they never returned. “Large treatment centers were being treated by the local population as death camps,” University College London’s Richards says. “People were dying alone, with no connection to the outside world.”
Distrust of these health officials naturally spurred speculation. Rumors began to fly that the centers’ stated function of treating people for Ebola was a scam—that the staff were harvesting patients’ body parts to make a profit.
With input from local teams in Sierra Leone, ERAP advised international responders to create a new clinic model: community care centers, which would be locally run, staffed with community residents, and free of intimidating features like tall barriers.
The new community care centers offered a different, more welcoming atmosphere. Though visitors could not cross into areas where there was a high danger of viral transmission, the open-plan design allowed relatives to see patients being treated through transparent panels or open-sided tents. Patients with possible Ebola symptoms were tested for the virus, but only those who tested positive—a relatively small fraction—were sent on to larger specialized health centers.
Still, Richards, along with Esther Mokuwa, a social scientist with Njala University, observed that many people, especially in rural areas, were shunning the hospitals and clinics. Richards advised first-response teams to develop a home-care protocol so people who were tending to their relatives at home could do so in the safest way possible.
Representatives of NGOs working in the area resisted those initial ideas, Richards says. “They said, ‘Unless this is being requested by the government, we’re not even prepared to discuss it.’” NGOs and public health responders in Sierra Leone feared home care would lead to viral transmission between family members.
These contentious exchanges dragged on so long that Mokuwa eventually told the chief medical adviser to the U.K. Aid Ministry: “There will be home care whether you like it or not.”
Mokuwa, who’d grown up in Sierra Leone, knew that many people felt sending their loved ones to treatment centers meant abandoning them. Her bone-deep knowledge—based on her own experience and her conversations with locals—spurred medical responders to move forward with solutions more in line with village realities.
Eventually, a variety of international aid providers, including the U.S. Centers for Disease Control and Prevention, developed protocols that allowed people to care for the sick at home in ways that minimized transmission risk. Informed by local populations’ experience in controlling past smallpox epidemics, the new home-care advice included quarantining Ebola patients in separate structures like huts and having one family member serve as primary caregiver so others in the household would not be exposed to the virus.
ERAP and SSHAP’s responses to cultural concerns around Ebola in African nations helped Wilkinson and her team create a blueprint—one that involved gathering cultural knowledge and building trust between communities and health care workers. As COVID-19 hurtled its way around the world in March 2020, the SSHAP team looked for ways to use this knowledge to help fight the new respiratory virus. The group’s efforts extend beyond Sierra Leone and the DRC: The core SSHAP team fields requests from first responders around the world, connecting them with local experts and social scientists.
Though COVID-19 is transmitted predominantly through exhaled aerosol particles—unlike Ebola, which spreads through direct contact with bodily fluids—both are dependent on how people interact. That means both can be managed with strategies that are responsive to people’s life circumstances and cultural backgrounds. To that end, experts in SSHAP’s broad networks are conducting their own coronavirus fieldwork in an effort to put local feedback at the center of discussions about epidemic and pandemic management.
In Dhaka, Bangladesh, Brac University medical anthropologist Sabina Faiz Rashid has zeroed in on challenges that residents of Dhaka’s informal settlements have faced since the pandemic began. These communities, known as bastis, dot the outskirts of the capital and are home to millions of people living below the poverty line. Rashid and her team interviewed several dozen residents of these dense urban settlements by phone, since city residents were under shutdown restrictions.
“You have to go to the source … to learn from their experience,” says social scientist Roland Suluku.
Rashid’s interviews paint a portrait of a community that largely understood the measures necessary to prevent infection. But people were running up against a series of practical and social barriers when they tried to put these measures into practice.
In the bastis, four or more people typically occupy a room about 12 square meters in size. Residents were often unable to adhere to the government’s distancing recommendations. A stifling climate of fear and stigma had arisen, Rashid learned, fueled by fines and other harsh measures that treated a COVID-19 diagnosis as a kind of scarlet letter.
“The government started putting red flags on houses that had COVID,” Rashid says. As a result, she adds, some people hid their symptoms and refused to seek medical care, accelerating the virus’ spread. “You have a fear of, ‘If I tell someone, maybe I’ll be picked up by the police.’”
Many bastis dwellers also felt that they had to choose between supporting their families and following public health guidelines. One woman told Rashid’s team: “Most of the community members are struggling financially during this pandemic. They can barely afford to eat twice a day. How will they buy soap for washing hands?”
What Rashid heard convinced her that Bangladesh’s government needs to roll out measures that meet bastis residents where they are, rather than holding them to sanitation standards that are impossible in their current situation. In her conversations with NGOs and policymakers, Rashid has argued for distributing financial aid to bastis dwellers and others in similar straits so that monetary concerns won’t threaten their adherence to public health guidelines.
At a global level, SSHAP scientists have issued a series of emergency briefings on COVID-19, some of which emphasize the twin Ebola-era goals of developing culturally sensitive home-care and burial guidelines—both of which have demonstrated their staying power in the course of global coronavirus response efforts.
SSHAP’s work joins a broader shift in public health, the impacts of which are visible in the COVID-19 response in multiple countries. In the U.S., the CDC recently published a detailed guide on home-based care for coronavirus, stressing that patients recovering at home should separate themselves as much as possible from others in the household.
First responders around the world have developed safe, dignified burial guidelines for COVID-19 victims modeled on those developed for Ebola. And following the success of locally supported ventures in response to Ebola, NGOs have enlisted local civic leaders in different countries to convey the importance of coronavirus control measures such as social distancing.
Among the most important lessons of Ebola is that a culturally informed response is a more effective one, which should motivate health officials to build social insights into epidemic and pandemic control as a matter of course. But most social scientists think their role in countries’ epidemic responses still has room to grow.
Richards fears some of the knowledge ERAP and SSHAP have shared with governments is already being lost. In his home country of Britain, he says, “you look at the advisory committee on COVID-19, and you see few observational social scientists.”
Wealthy countries such as the United States have much to gain from socially literate epidemic and pandemic management, as former CDC anthropologist Robert A. Hahn observes. The cultural realities of COVID-19 in the U.S.—the religious opposition to bans on large gatherings, the rejection of mask-wearing to signify political loyalties—constantly run up against health teams’ attempts to stem transmission.
UNICEF epidemiologist Simone Carter, a SSHAP collaborator, points out that health workers need to communicate with people on the ground to understand real-world barriers to controlling disease. “Have a conversation with them,” she says. “You don’t need a study. You have community engagement teams who should be able to tell you what’s happening.”
Suluku concurs. “You have to go to the source. … You have to understand the dynamics—to learn from their experience.” To that end, the U.S. National Science Foundation recently announced a US$200,000 Rapid Response Research grant to University of California, Irvine, researchers who are studying how U.S. communities’ perceptions of COVID-19 risk affect how they protect themselves from infection.
Just as in Sierra Leone, the DRC, and Bangladesh, health officials in every nation now have the chance to tap into people’s deepest values and fears to develop epidemic and pandemic control strategies that respond to them—and that accomplish the broader goal of stopping viral spread.
“When you have a very biomedical response, you miss cultural opportunities to do adequate risk communication,” Rashid says. “Context matters. It’s really important to learn from other countries, learn from each other.”