Gene Therapy’s Promise Meets Nigeria’s Sickle Cell Reality

“DON’T PLAY WITH HER! SHE HAS SICKLE CELL”
On a sunny day in Southern Nigeria, my uncle and aunt took their children to the hospital. Because their daughter had suffered swollen joints and body pains for months, a doctor advised genetic testing. The results diagnosed her with sickle cell anemia, a genetic blood condition characterized by defective hemoglobin, the protein in red blood cells that ferries oxygen around the body.
In the 15 years since her diagnosis, my cousin has undergone multiple blood transfusions and debilitating pain crises. Throughout her life, she has been described by relatives as “unwell” and “frail.” Her parents and teachers prohibited her from play and physical exertion. Kids made fun of her for being sick.
My family and I are relieved that she is alive.
Millions of people worldwide live with sickle cell anemia, although an exact count remains elusive due to factors such as underdiagnosis, underreporting, and early deaths. In Nigeria, an estimated 1 in 4 individuals bear the sickle cell trait.
As a medical anthropologist, I am interested in how the condition influences families and relationships. Beyond the physical pain caused by sickle cell disease lies mental health battles, social stigma, and financial strain, which often silently impact patients and families.
In December 2023, the U.S. Food and Drug Administration approved two gene therapies for treating sickle cell disease—one that uses gene editing to alter patients’ DNA and another that uses the body’s cells to produce sufficient anti-sickling hemoglobin to reduce or stop pain crises. Considering the procedures may cost around US$2.2 million per patient, the breakthroughs will provide little relief in Africa. The promise of this advancement rings hollow when financial barriers lock out those who need it most.
More practically and immediately, the lives of many millions could be improved by social changes aimed at reducing stigma and enhancing accommodations for those who bear sickle cell disease.
SICKLE CELL ORIGINS
Being Nigerian, my family is not exempt from sickle cell’s impacts. Growing up amid this ailment fueled my curiosity to learn more about it. How do the sickle-shaped cells form? What mental, social, and economic tolls do patients and their families bear? What measures can prevent the disease from passing on to the next generation?
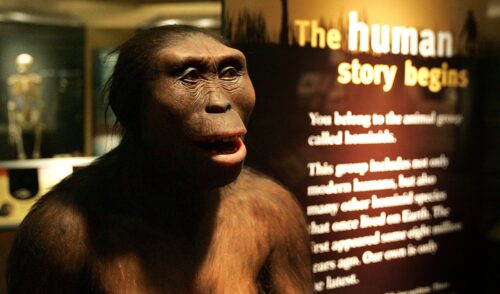
The sickle cell genetic mutation first appeared in Africa thousands of years ago. Over generations, the DNA change became more common because it provided some resistance to malaria, the leading killer on the continent until the 21st century. Still a potentially deadly illness, particularly for young children and pregnant people, malaria is caused by Plasmodium parasites and transmitted by bites of infected Anopheles mosquitos.
While malaria is often associated with tropical and subtropical regions, it can affect anyone in contact with infected mosquitoes. However, there are variations in genes that have been linked with resistance to malaria. Everyone carries two versions of this gene—one inherited from each parent.
Compared to individuals with two “normal” copies, a person with one normal and one sickle cell–causing version has a tenfold reduced risk of malaria. This is because sickle cell hemoglobin carries less oxygen, and low oxygen impairs Plasmodium growth in red blood cells. In addition, compared to normal red blood cells, sickle cells die earlier and get removed from the bloodstream faster, along with the parasites.
But individuals with two disease-causing versions are likely to have sickle cell anemia, which can lead to death. Today most sufferers receive treatment, but they may still experience fatigue; swelling of the hands and feet; stunted growth; episodes of bone pain; recurring infections; severe conditions of the kidneys, lungs, muscles, and skeleton; and a variety of associated illnesses.
Before it was recognized in U.S. and European medicine, sickle cell disease was known in numerous societies in Africa. Children with the sickle cell trait were labeled abiku (“predestined to die”) among the Yoruba of Southwestern Nigeria, and ogbanje (“one who comes and goes”) by the Igbo of Southeastern Nigeria.
In both these cultural traditions, children were believed to have been sent from the spirit world to plague their parents. To ensure the children stayed in the land of the living, parents offered sacrifices to gods. But the children often died before they turned 5, mostly from harmful concoctions and charms, which were believed to vanquish death.
MEDICAL STUDY AND TREATMENTS
Sickle cell anemia was first documented in medical literature in 1910. At the time, scientists knew little about the disease’s cause besides its characteristic sickle- and crescent-shaped red blood cells.
In 1949, British-Indian scientist J.B.S Haldane formulated what is now known as the “malaria hypothesis.” He noticed the prevalence of abnormal red blood cells in tropical areas, where malaria was also common. Linking the two, he proposed that natural selection favored the sickle cell trait because it protected people from malaria. This hypothesis was confirmed in 1954 by Anthony C. Alison, a Kenyan geneticist and medical scientist, who analyzed blood samples of Kenyans.
In the 1960s, medical staff began using blood transfusions to treat patients with sickle cell disease. Since then, more advances have improved the lives of those with the disease. Until recently, the sole cure was a stem cell transplant, requiring bone marrow from a donor. This treatment can’t help everyone, though: Compatible donors can be rare, and patients’ immune systems sometimes reject the transplant.
A novel cure now exists through the first gene therapies for sickle cell disease. These treatments modify the DNA within the patient’s cells, allowing them to generate a different version of hemoglobin. But their price tags of well over US$1 million renders the treatments unattainable for most families in Nigeria, where the average annual income is below US$9,000.
How then can sickle cell disease be effectively treated or eliminated?
SOCIAL SOLUTIONS
For centuries, patients in Nigeria have managed sickle cell anemia with herbs such as garlic bulbs, cloves, West African black pepper, unripe papaya fruit and leaves, pumpkin leaves, and a variety of others. I have researched some of these plants, and while some do elevate hemoglobin levels and reduce blood cell sickling, they do not cure the disease and could even be harmful.
Patients and their families cope through other means such as prayer. To protect their sickle-cell diagnosed children, parents often forbid strenuous or dangerous activities. They may urge teachers to take extra care of their kids, which can cause isolation or embarrassment.
Many adults with sickle cell anemia, alongside religious organizations, have begun taking deliberate actions to guarantee that children do not suffer the same fate as parents with the disease. Now more common and affordable in Nigeria, genotype testing and counseling allow couples to make informed decisions about their genetic risks.
But such tests only help reduce the disease counts in future generations. For those already living with sickle cell, the immediate physical symptoms are compounded by the consequences of ostracism. Sickle cell disease affects the mental health of the patients, their relationships, and their sense of self within their families and communities.
Children with sickle cell disease experience greater social restrictions, self-esteem issues, and fear of underachievement. Depression often afflicts adolescents, who worry about their prospects for careers and romance.
My cousin, for one, can attest. The constant pain, fatigue, and uncertainty about the next crisis at times has plunged her into long periods of depression.
Sickle cell anemia cannot be eliminated with state-of-the-art medical treatments only available to the privileged. The burden of disease shouldn’t be borne alone by patients and their loved ones. Government and communities have a responsibility to make living with sickle cell bearable—even convenient. Organizations leading this effort include the Sickle Cell Foundation Nigeria, Sickle Cell Hope Alive Foundation, and several other nongovernmental organizations.
In recent years, awareness of the disease has improved in Nigeria. People with sickle cell have begun to speak out about how they have been treated differently and made to feel as if they cannot be productive, “normal” people. In additional to accessible medical care, successful sickle cell treatment requires inclusion, empathy, and a web of support.