Can Medical Anthropology Solve the Diabetes Dilemma?

Mary (a pseudonym) was 18 years old and halfway through her second pregnancy when anthropologist Carolyn Smith-Morris met her 10 years ago. Mary, a Pima Indian, was living with her boyfriend, brother, parents, and 9-month-old baby in southern Arizona. She had been diagnosed with gestational diabetes during both of her pregnancies, but she didn’t consider herself diabetic because her diabetes had gone away after her first birth. Perhaps her diagnosis was even a mistake, she felt. Mary often missed her prenatal appointments, because she didn’t have a ride to the hospital from her remote home on the reservation. She considered diabetes testing a “personal thing,” so she didn’t discuss it with her family.
As Smith-Morris’ research revealed, Mary’s story was not unique among Pima women. Many had diabetes, but they didn’t understand the risks. These women’s narratives have helped to explain, in part, why diabetes has been so prevalent in this corner of the world. An astonishing half of all adult Pimas have diabetes.
Medical anthropologists like Smith-Morris are helping the biomedical community untangle the social roots of diabetes and understand how and why the disease is exploding in the United States. Smith-Morris, based out of Southern Methodist University in Dallas, Texas, has been working on this cause for over 15 years—from a decade spent among the Pimas, to a new study sponsored by Google aiming to prevent diabetes-related blindness. Anthropology, she says, provides the most holistic perspective of this complex problem: “Anthropology seems to me the only discipline that allows you to look both closely at disease … and from the bird’s eye perspective.”
More than 30 million people in the United States are estimated to have diabetes, and it’s on the rise. If trends continue, 1 out of every 3 American adults could have diabetes by 2050, according to the Centers for Disease Control and Prevention.
The condition involves insulin, a hormone that regulates the way the body uses food for energy. In type 1 diabetes, the body stops making insulin entirely; those affected need daily insulin injections to survive. In type 2 diabetes, which accounts for the vast majority of cases, change is more gradual. The body slowly makes less insulin and becomes less sensitive to it over the years. Gestational diabetes, which strikes during pregnancy, can give mothers a dangerous condition called preeclampsia, which is related to high blood pressure and can harm both mothers and babies. Women with gestational diabetes are more than seven times likelier to later develop type 2 diabetes than women who do not have the condition in pregnancy, and their children are at higher risk of obesity and diabetes. If left untreated, diabetes can cause heart disease, kidney failure, foot problems that can lead to amputation, and blindness.
The preventative measures for type 2 and gestational diabetes are seemingly straightforward: eat healthy foods, lose weight, and exercise. Treatment for both can include taking medications. Yet prevention, lifestyle, and treatment cannot entirely solve the problem; family history, ethnicity, and other factors play a critical role in a person’s susceptibility to type 2 and gestational diabetes. Both forms of diabetes continue to plague Americans, particularly certain groups, including Native Americans. “My interest in diabetes grew out of an interest in Indigenous groups,” says Smith-Morris. “I took on diabetes because it was important to them.”
From 1965 to 2007, the Pimas of Arizona were the focus of the largest continuous study of diabetes in Native Americans. Conducted by researchers from the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), it examined the environmental and genetic triggers of the disorder, management of the disease, and the treatment of thousands of Pimas. It also documented that they had the highest prevalence of diabetes ever recorded. The pivotal work told researchers much of what they know about diabetes today, including that obesity is a significant risk factor, and that a mother’s diabetes during pregnancy can pass risk along to her children.
The political and economic contributors to the Pima people’s health problems have long been well-known: Their traditional farming practices collapsed during the late 1800s and early 1900s when non-Native settlers upstream diverted essential water resources, contributing to poverty, sedentariness, and a lack of fresh food. Yet Smith-Morris felt something integral was missing from this picture: the Pimas’ stories.
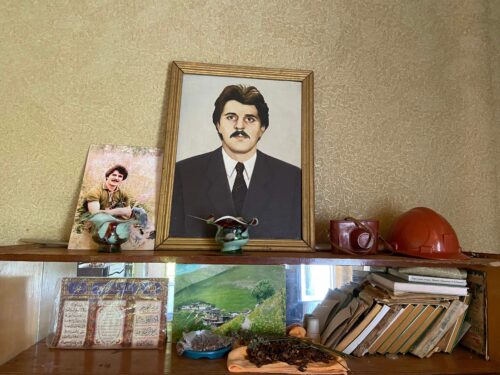
In 1997, Smith-Morris stayed among Pima women and their children to fill in that gap. (Her research was independent from the NIDDK project.) Her work was the first to share the voices of women as they dealt with diabetes during their own pregnancies, and coped with the horrible effects of diabetes, such as amputation and blindness, among their families. She interviewed 90 people between 1999 and 2000 in their living rooms, kitchens, and backyards; she attended birthday parties, family memorials, fitness walks, and cooking classes. She even drove women to their prenatal appointments. Smith-Morris was pregnant at the time, which helped her get close to women who didn’t really want to talk about their health with outsiders. “Despite decades of research on the topic here, Pimas remain reactive, reflective, and very private about this disease,” she wrote in her 2006 book, Diabetes Among the Pima: Stories of Survival.
Smith-Morris’ work highlighted how unhealthy foods, such as fry bread, had become an integral part of social and religious gatherings for the Pima people, noting that these foods were even seen as the mark of good cooking. Fresh foods are expensive and hard to find on the reservation, Smith-Morris notes. It’s also incredibly hot in the Sonoran Desert, with summer temperatures regularly exceeding 100 F, making it uncomfortable for many pregnant women to cook or exercise.
Many women felt that diabetes was somehow inevitable because of their community’s long history with the disease, Smith-Morris found. And yet it also carried a stigma, making its diagnosis and treatment challenging.
In 2002, while Smith-Morris was still living among the Pimas, there was good news in the world of diabetes. A landmark study called the Diabetes Prevention Program (DPP) showed that people at risk for developing diabetes could delay or prevent the disease through modest changes to their diet and level of physical activity: Losing 7 percent of their body weight decreased their risk of diabetes by 58 percent. Some Pimas were part of this study, which took place in 27 clinics across the country from 1996 to 2001.
Smith-Morris says she saw the positive impact of the program firsthand: She saw Pima women participate in the DPP and then keep up their new dietary and exercise routines even after the program ended. She saw the tribe invest in fitness centers, and find new ways to educate and treat people with diabetes outside the hospital through community-based nursing and casework. The fact that the Pima people live in a small community with control over their own funds for things like public health helped them to take action quickly, Smith-Morris notes.
Things have improved for the Pima people, who, together with the Maricopa tribe, make up the 11,257 strong Gila River Indian Community Reservation outside of Phoenix, Arizona. According to the NIDDK, from 1975 to 2004 the Pimas’ health steadily improved, specifically in terms of blood glucose, blood pressure, and cholesterol. In 2007, the Pimas decided to decline further outside research of their community in favor of community-led studies and interventions.
It’s difficult to see how the work of researchers like Smith-Morris has made life explicitly better for the Pimas: “It’s hard, if not impossible, to quantify,” Smith-Morris admits. But others note that this kind of work has proven vital in highlighting the importance of social factors in disease. Steve Ferzacca, an anthropologist at the University of Lethbridge in Alberta, says that work like Smith-Morris’ with the Pimas turned public attention to the role that changes in diet may play in the rise of diabetes all over the world, as people in Westernized cultures eat more processed foods.
Today, community-based diabetes programs have popped up throughout the U.S. For example, the Young Men’s Christian Association (known as the YMCA or Y) is a community service organization that has its own Diabetes Prevention Program based on the same diet, exercise, and weight loss strategies used in the DPP study published 15 years ago. Participants go to 25 one-hour, small-group sessions with a lifestyle coach over the course of a year. They learn to eat healthy foods and to exercise at least 150 minutes a week. More than 53,000 people have participated in the program at 1,699 sites in 47 states, with an average weight loss of 5.5 percent.
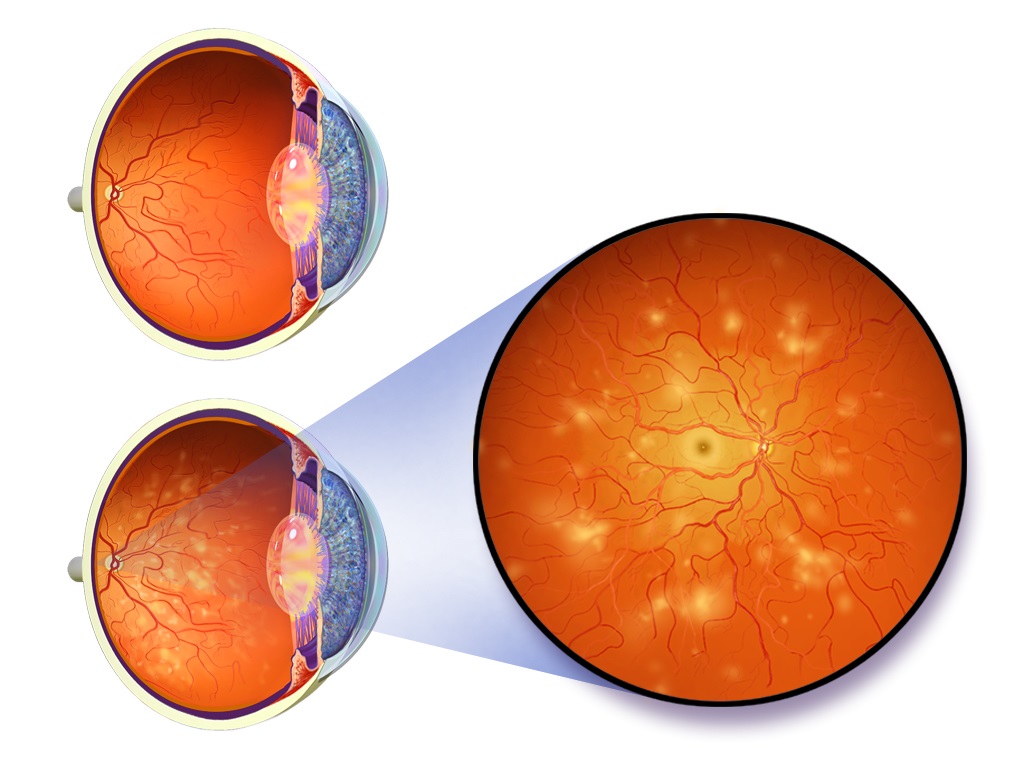
Today, Smith-Morris is still trying to work out how and why some populations continue to struggle to manage diabetes and its complications. Her latest project in community health clinics has been with optometrist Jorge Cuadros, who is trying to improve early detection of diabetic blindness; doctors can prevent diabetic vision problems 90 percent of the time if they detect and treat eye disease early with injections or laser surgery. “Most people with sight-threatening retinal disease wait until it’s too late,” says Cuadros. “That’s why diabetes is still the main cause of vision impairment and blindness in working age adults in the United States.”
In 2010, Cuadros founded a company called EyePACS that deploys cameras and trains technicians to take photos of people’s eyes. Most of their work so far has been in community health clinics. Photos are uploaded to the EyePACS website, where eye specialists evaluate them and make recommendations for treatment. Google has gotten involved too, developing computer algorithms that can automatically flag retinal damage in these photos. Since it started, EyePACS has screened over half a million people, most of them with diabetes.
But in follow-up studies, Cuadros realized that many of the people with early signs of eye damage were falling through the cracks. In studies of clinics in 2009 and 2010, he and his team found that less than a quarter of patients with sight-threatening eye disease had received treatment. “What are the factors that keep people from getting treated? That’s the bottom line,” says Cuadros.
And that’s when Cuadros and his EyePACS collaborator ophthalmologist George Bresnick called in Smith-Morris, hoping a medical anthropologist could dig into people’s lives and figure out how to help. Smith-Morris and anthropologist Kathryn Casey Bouskill, now of the RAND Corporation in Santa Monica, California, started talking with medical staff and patients, both at clinics and in their homes. “The work that Carolyn did tells us how difficult it is to be able to follow instructions that we, as providers, think are really easy,” says Cuadros. Patients face significant barriers such as work commitments, social isolation, and transportation and other logistical issues, as well as time-consuming tasks like waiting on hold to make an appointment.
Perhaps the biggest barrier the anthropologists uncovered is that patients don’t always believe treatments work, or are necessary. “It’s becoming increasingly clear that patients don’t follow instructions,” says Cuadros.
Diabetic eye disease often progresses without affecting vision, so patients may not believe they are at risk for going blind. Identifying these beliefs allowed Cuadros and his team to home in on a central message to their patients: Even though you may be seeing well now, you need treatment to avoid going blind in the future. That message must be repeated early and often by providers in the clinics that EyePACS serves, says Cuadros.
This conclusion also spurred EyePACS to change course slightly, working to develop a system that can document stages of disease rather than solely provide a simple thumbs-up or thumbs-down diagnosis. In this way, patients can see more clearly that the problem progresses, even without obvious symptoms to mark the progression.
“As an optometrist and health care provider, I don’t understand as well as social scientists what happens outside the exam room,” says Cuadros. “We need social scientists to guide us so that we can develop systems of care and interventions that will actually prevent vision impairment and other complications.”
It is unusual, say both Smith-Morris and Bouskill, to find doctors like Cuadros and Bresnick, who look past biomedicine to the realities of their patient’s lives. A holistic perspective about the disease is vital, says Emily Mendenhall, an anthropologist at Georgetown University in Washington, D.C., who also studies diabetes. “There is no other way,” she says. “Stress and chronic, untreated depression, racism, and poverty—all these are closely tied to diabetes.” Experts agree that all of these factors need to be understood in order to assess the value of proposed solutions. A tax on soda pop, for example, might deter people from drinking too much of the sugary drink, but it also empties pockets and increases poverty-related risks.
“Diabetes is an expression of culture,” says Smith-Morris. “It’s how people live. It’s an expression of their dietary choices. It’s an expression of their genetic makeup. It’s an expression of whether they exercise or not. What their values are in life.” And, she adds, “As anthropologists, that’s really what we’re interested in, the full wide context in which people live their lives and make decisions.”