The Birth Whisperers of Timor-Leste

Rosa Bana rolls the cuffs of her jeans up to her knees. She grabs a couple of water bottles and drapes a jacket over her head to shield herself from the piercing sun. It’s five hours up the mountain by foot (or three hours by car, if there is a car, but that’s rarely the case). Kutete, her village of 150 households, sits more than 2,000 feet up a mountain in this remote enclave of Timor-Leste. Sheer drop-offs and deep valleys characterize this whole island, a rugged landscape comprising a bit of Indonesia and the nation formerly known as East Timor.
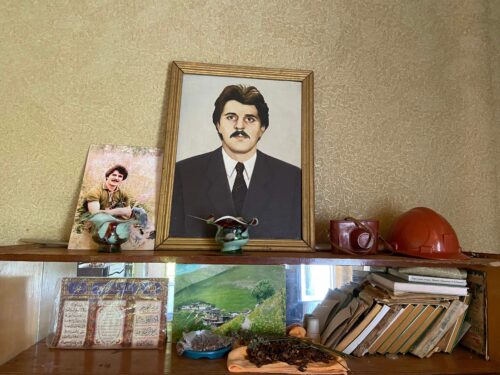
Bana makes the trek down and back up to Kutete at least once a month—sometimes once a week—to fetch supplies. She is the only trained community birth attendant (CBA) working in the village and nearby region; she serves the hundreds of women in five villages scattered across the mountain, and some in neighboring Indonesia. Everyone calls her “Mana Rosa,” an affectionate term that means sister. For tens of thousands of Timorese women, a birth attendant like Mana Rosa is their only link to medical care.
It’s midafternoon on a hot day in October 2015, and we are the only people on the road: Mana Rosa; Sidalia do Rego, who is coordinator of women’s health and social care at the clinic where Mana Rosa trained; my husband (a photojournalist); and me. The air is dense with heat and smoke from agricultural fires. It hasn’t rained in months, and El Niño has delayed the onset of monsoons. The sun pummels us as we shuffle up the steep incline, stopping to rest in the slim shadows of any available bush.
Mana Rosa is 27 years old and has lived her entire life in Oecusse, a district of 314 square miles and 72,000 people stranded like an island in the middle of Indonesian territory. It takes hours by boat or car to reach the rest of Timor-Leste from Oecusse. In 2012, Mana Rosa’s community selected her as a potential birth attendant because she was widely liked and trusted. To fulfill the role, Mana Rosa traveled to the Bairo Pite Clinic in Dili, the country’s capital, more than 120 miles to the east of her home, to study the fundamental skills of birthing attendance—at no cost and for no pay.
Mana Rosa was nervous at first. She hadn’t attended much school, and she didn’t speak Tetum, one of the official languages of Timor-Leste (along with Portuguese), so she had to learn it. She also didn’t have experience with childbirth. “I was afraid,” she tells me, with do Rego translating. (Do Rego serves as my translator throughout this trip. Her first language is Tetum, but she also speaks fluent English. Mana Rosa’s first language is Meto, which is spoken throughout Oecusse. She and do Rego communicate through multiple languages. Interviews with Kutete residents are a bit tricky: I ask questions in English, do Rego translates to Mana Rosa, who translates to the interviewee. The answer comes back to me through at least three languages, sometimes more.)
Three months after boarding a boat for Dili, Mana Rosa passed an oral and written exam. Upon graduation, she received an equipment bag filled with the things she might need and that the women of Kutete didn’t usually have: everything from a battery-operated fetal heart monitor to sterile blades and soap. Then she went home to work.
Kutete has no doctors, midwives, or emergency services. Before her training, “there was no one to assist pregnant moms,” Mana Rosa says. “Just the family helped out.”
Every day, more than 800 women die worldwide in complications from pregnancy and childbirth. That’s down 44 percent since 1990—a significant improvement, but maternal mortality remains “one of the world’s most neglected problems,” according to the United Nations Population Fund, an agency that works to improve global reproductive health. “The reality for upwards of 50 percent of women in the world today: No access to [a] skilled birth attendant, no access to a facility,” says Margaret MacDonald, a York University medical anthropologist who researches midwifery and global campaigns to improve maternal mortality rates. Women in undeveloped, rural areas are at greatest risk.
And Timor-Leste consistently ranks among the world’s riskiest places in terms of overall health, due in part to its turbulent past. The country became independent in 2002, following 24 years of Indonesian occupation and 450 years of Portuguese colonization before that. The Indonesian period was particularly brutal: More than 200,000 Timorese died in massacres and attacks that many consider genocide. When the Timorese overwhelmingly chose independence in a 1999 referendum, a rash of violence before and after the vote left thousands more dead and much of the country in ashes. The fighting obliterated roads, schools, and hospitals, and the devastation exacerbated the pre-existing problems of a rural, impoverished population.
Today the infant mortality rate in Timor-Leste is among the worst in Asia: 45 per 1,000 live births—nearly 8 times that of the United States and 23 times greater than Sweden’s. The maternal mortality ratio, which varies widely depending on the source, is equally troubling.
Aside from the country’s difficult history, many other factors put Timorese women and newborns at risk. About 70 percent of the population lives in isolated mountain villages. Women typically give birth at home, with help from relatives who have no medical training. Water is not always available, equipment is often unclean, and the umbilical cord is often cut with unsterilized bamboo. Many roads are impassable during the monsoon season, and no one in Kutete owns a car anyway. “When it’s rainy, no cars will pass through here—not even the motorbike,” Mana Rosa explains. Few areas have an ambulance, and it can take hours to get a woman to the hospital at the base of the mountain.
Consequently, improving maternal health is both a high priority and one of the country’s biggest medical challenges. In 1999, an American doctor named Dan Murphy founded the Bairo Pite Clinic to provide general health care and, eventually, a safer environment for births. In 2005, the clinic took on the extra task of training local women to work as CBAs in their own villages.
Their goal is simple: “Ensure that all women in the community are cared for by a trained health care worker,” says Sarah Moulton, an Australian clinical nurse midwife who wrote the Bairo Pite CBA training manual and conducts annual refresher courses. Each candidate learns to provide care before, during, and after delivery. Students also learn when to refer a woman to a doctor if things start to go wrong. “The women who come for training actually receive input 24/7, as they live in the staff room in the maternity unit,” Moulton says. “They are involved with anyone who is in labor, no matter what the time.”
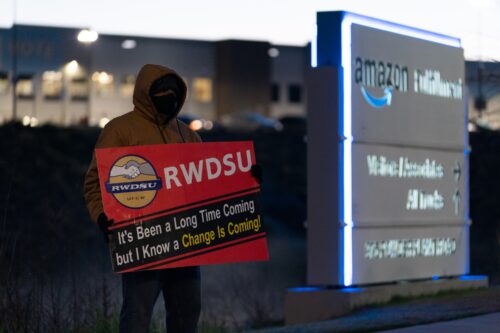
Training local birth attendants is not a new idea, but it has a complicated history. In 1987, the World Health Organization (WHO) launched the Safe Motherhood Initiative, which was a groundbreaking global effort to tackle maternal mortality, says MacDonald. A key component of it was to provide some medical skills to traditional birth attendants (TBAs)—the people, mainly women, already accustomed to helping out with births in a community. But “the toll on maternal mortality did not budge,” MacDonald says. Research shows that many TBAs did not get the medical support or equipment they needed, and improved birthing strategies were not always put into practice. So the WHO changed its tack. The new focus became getting people with a higher level of training—skilled attendants such as doctors, nurses, or midwives—into communities that needed them.
But there have long been problems bridging language and culture divides between accredited health professionals and local communities. (Timor-Leste, for example, is an ethnically diverse country with more than a dozen Indigenous languages and cultures.) The Bairo Pite program tries to overcome these hurdles by giving reasonably good skills to locals who work in their own communities. They know the language and often are able to provide emotional support in ways that outsiders cannot. Bairo Pite offers annual refresher courses for CBAs, and the clinic fosters an ongoing relationship with workers like Mana Rosa long after their initial training. This is the most consistent form of medical attention many rural Timorese mothers have ever had.
It’s nearly dark by the time we reach Kutete. Sometimes, Mana Rosa says, she walks most of the night to reach the women in her care. She usually has a flashlight, but a dog recently mauled it, so she uses the light on her phone. We’re exhausted. We stop to eat a dinner of rice and tempeh (fermented soybean cake) before falling asleep. Mana Rosa plans to show us her village in the morning.
She rises around 4 a.m., before the sun. After a breakfast complete with strong Indonesian coffee, we follow her uphill to the community health office, a one-room, concrete box with a covered front porch, which shares a property with the elementary school. Mana Rosa collaborates with a handful of community health care volunteers—like her, all are unpaid. The volunteers grow corn, cassava, and vegetables, subsisting on the little money they earn from farming, just as Mana Rosa’s family does. They received basic training at an Oecusse hospital, and they work through a nationwide Integrated Community Health Services (or SISCa) program aimed at providing primary health care to rural communities.
A few minutes after we arrive, two volunteers appear—35-year-old Estefanos Queno and 45-year-old Marcos Lasi, chief of volunteers. They invite us inside the concrete room to see their equipment: two wooden cabinets with bandages, scissors, scales, a few alcohol swabs, and little else. Diarrhea is rampant, Lasi says, but “I have to go all the way to town just to get the meds.” That’s a full day round trip by foot.
Do Rego says volunteers are supposed to be in regular contact with the district health system, which is based down the mountain. But that isn’t always the case. The SISCa is supposed to offer regular checkups, vaccinations, and other screenings with the help of district health workers who travel to Kutete on a regular basis—but “November to June they stop because of the rainy season,” Mana Rosa explains. Plus, the volunteers in Kutete have cellphones—but not always the money to use them. As a result, “the community health workers are kind of stressed out,” she notes. They have minimal supplies, little contact with other health workers, and a lot of worries on the job.
Mana Rosa has a mantra that she repeats in Tetum to keep her going during the tough days: “Forsa, forsa, forsa.” Strong, strong, strong.
After we leave the community health post, we head to her home, where we see the record book noting every pregnancy she has attended: more than 100 since 2012. She recalls one of the scariest births, in July 2015. A friend of hers went into labor, the baby was breech, and Mana Rosa struggled to get the baby out safely. She called her priest, who phoned the hospital down in town. It was Sunday, and the only ambulance was in another town far away. So Mana Rosa called her brother, who searched for someone—anyone—with a private car. He found a man who sent a vehicle to Kutete, which transferred the woman to the hospital, where she had a cesarean section. Both mother and baby survived.
Mana Rosa says she hears of a few newborns dying every year, but so far it hasn’t happened to her. “Before, I was afraid,” she says. “Now I am brave, and I want to do more.”
Mana Rosa spends a lot of time talking with women about what they eat. Malnutrition is chronic in Timor-Leste: 21 percent of females aged 15 to 49 are anemic, 38 percent of the population is malnourished, and 58 percent of Timorese children under the age of 5 are stunted—the highest rate in the world. People will often grow vegetables or raise chickens and eggs for sale rather than for eating—because they need the cash or because they don’t understand what the body needs for a balanced diet. Husbands will often tell their wives to sell the food, leaving women little say in what they and their children eat. “Not many people eat fruit,” do Rego adds. “They don’t think it’s important.” Yet papayas, mangoes, and bananas grow like weeds.
In many parts of the country, cultural prohibitions on eating certain foods during pregnancy can exacerbate malnutrition, says Rosaria Martins da Cruz, director of a nongovernmental organization (NGO) in Dili called HIAM Health, which stands for Hamutuk Ita Ajuda Malu in Tetum (Together We Help Each Other). Some pregnant women avoid eating eggs, prawns, or fish. “This is part of our culture,” passed down through generations, da Cruz says. While uncooked eggs and seafood can pose risks to expectant mothers, cultural prohibitions like these can prevent women from getting the protein they need. Part of Mana Rosa’s job is to educate women about the importance of nutrition. “We ask the mother to breastfeed and eat some good food,” Mana Rosa says.
Cultural factors come into play during and after birth as well. It is Timorese tradition to keep mothers near a burning fire after labor; throughout many rural parts of Southeast Asia, it is believed that heat expels bad blood and wards off disease. New mothers are expected to drink and bathe in hot water. Hot coals are often placed beneath their beds. Some Southeast Asian women are forced to sleep above a fire. These practices can lead to burning, dehydration, and other serious health problems. Mana Rosa says she doesn’t see this much in her area, but it is an issue for other health workers in Timor-Leste.
Globally, many cultures have pregnancy and birthing traditions that are perhaps rooted in logic but explained through legends and stories. For example, it’s common for women in many parts of the world to refrain from revealing a pregnancy in the first three months. This makes scientific sense, MacDonald says, because statistics show that a pregnant woman is more likely to miscarry before 12 weeks. In Senegal, where she has worked, people also say that if a woman exposes her pregnancy early on, bad spirits could harm the fetus. Keeping the pregnancy secret, however, presents a health challenge. “How can you get someone into prenatal care if she hasn’t disclosed her pregnancy?” The solution, MacDonald says, is a program that works within the culture. Rural Senegalese communities have started forming all-female “care groups” in which a woman can freely reveal her pregnancy to the other members—but she doesn’t need to tell anyone else in the village. The woman is then paired with a godmother, who accompanies her to prenatal health visits.
Overcoming cultural barriers to achieve better maternal health is only possible when the community deeply trusts its health care workers and birth attendants. A critical part of the WHO’s efforts to lower infant and maternal mortality is to ensure that the skilled providers are both trusted in the local community and integrated with the formal health care system. “That means relationships have to be built,” says MacDonald. Birth attendants—locals or outsiders—must gel equally well with local health care providers and local communities. Just as Mana Rosa does.
Everyone I ask talks of Mana Rosa’s critical role in the community. “If Mana Rosa is around, I am going to call her!” says Julieta Kebo, a 25-year-old woman who is pregnant with her third child. (Mana Rosa delivered one of Kebo’s girls; she was in Dili for training during the birth of the other.)
We chat with Kebo in the shade of a wooden lean-to near her house. This is her first checkup with Mana Rosa, and she knows virtually nothing about this pregnancy. Kebo thinks she might be eight months along (though her belly barely shows). Twice, she says, she visited a clinic in another area, and the staff did nothing. They did not confirm the pregnancy, or test for HIV or hepatitis B—routine prenatal screenings. It’s unclear why they didn’t, but Mana Rosa isn’t surprised.
Both Mana Rosa and NGO workers in Dili talk about the discrimination, condescension, and stigma that rural women face—due to their poverty and/or lack of education—when visiting health facilities outside their home villages. While some women across Timor-Leste meet regularly with nurses or midwives and communicate with their local health workers via text messages, women who live in remote areas, like Kutete, can end up going through pregnancy alone. Kebo says the clinic told her to return in a month to get the standard booklet for expectant mothers, which tracks due dates, measurements, vitals, and other pertinent information. Instead, Kebo saw Lasi, who called Mana Rosa.
Women like Kebo often spend the months before labor working and living much as they always do—without extra support or attention. But childbirth is a different story. Women everywhere have always sought help when it comes time to deliver a baby.
Research shows that childbirth for humans is a uniquely social affair. “If you look at other primates,” says University of Delaware anthropologist Karen Rosenberg, “they all give birth in isolation. … Humans do exactly the opposite.” As humans developed intelligence and the ability to walk on two legs, birth became harder. “Our babies have large brains that have to fit through the birth canal,” she says. The back of the baby’s head is the wider part, so human babies typically come out facing away from the mother and are difficult for her to lift, Rosenberg notes. Humans have evolved to require help during labor.
Over time, Rosenberg says, some societies have “emphasized the medical part of childbirth assistance at the expense of the social and emotional part.” The latter are just as important, she says. Rosenberg points to research showing that women who give birth in the presence of a doula—a trained birth assistant who offers physical and emotional support—have statistically shorter labors and lower rates of cesarean sections. Women need both medical and emotional support during childbirth, she says. “I think it’s perfectly possible to do both.”
There are many ways to accomplish this—through doctors, relatives, doulas, and midwives. The CBAs are meant to fulfill both roles in places where help is in short supply. As a lifelong Kutete resident, Mana Rosa knows the women in the region well. Her training gives her medical skills; her character gives her clout.
Since 2005, the Bairo Pite Clinic has trained a few dozen CBAs from around Timor-Leste. Does their program work? There are no hard data. “We have not done any formal studies,” Moulton says, citing time and financial restraints. But anecdotal evidence shows that women now seek out a CBA rather than relying solely on the matriarch of the family, she explains. “We also know that the Ministry of Health has become more accepting of the role of CBAs in the community, as these are local women who speak the right dialect and are always there,” unlike health workers who are sent to a community but have no “connection to the people.”
In general, the WHO’s push for skilled birth attendants coincides with improved maternal and infant health rates. Globally, both maternal and infant death rates have dropped substantially in the past 25 years. But WHO acknowledges that these data might be skewed by the fact that many maternal deaths go unrecorded. The organization is on a mission now to monitor and improve global maternal death data.
As we hike back down the mountain with Mana Rosa, we follow a shady trail that crisscrosses a stream, over boulders and down steep, slippery cliffs. It’s much cooler than the road we took to Kutete—but steeper, too. We grip vines and trunks to keep from falling. Mana Rosa removes her shoes and descends barefoot for most of the three-hour hike.
She is always 10 steps ahead of us, humming soft tunes and chanting her mantra: “Forsa, forsa, forsa.”
Reporting for this story was made possible by a fellowship from the International Reporting Project.