A Native Alaska Community’s Reckoning With Vaccine Hesitancy

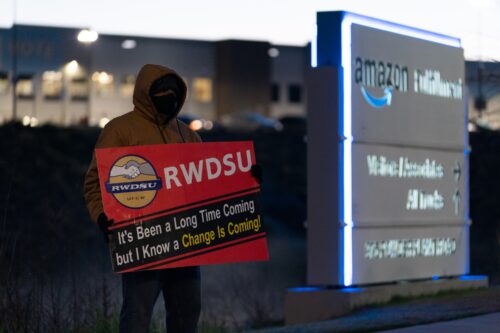
New COVID-19 boosters are now available in the U.S., freshly retooled for omicron subvariants. But booster uptake has been abysmal; only 13 percent of people above the age of 5 have gotten one since the bivalent vaccines first became available in October. Calls by public health experts asking the public to roll up their sleeves and get the vaccine have largely been ineffective.
Why do so many people remain hesitant to receive vaccines, despite strong evidence they save lives?
The answers are complicated, but understanding more about a community’s past is a good place to start. I’m a medical anthropologist who studies the history of infectious diseases among Tlingit people in present-day Alaska. My research has revealed one major roadblock to addressing vaccine hesitancy in the U.S.: Broadly speaking, many public health officials don’t know how the history of white supremacy has shaped people’s mistrust of the medical system.
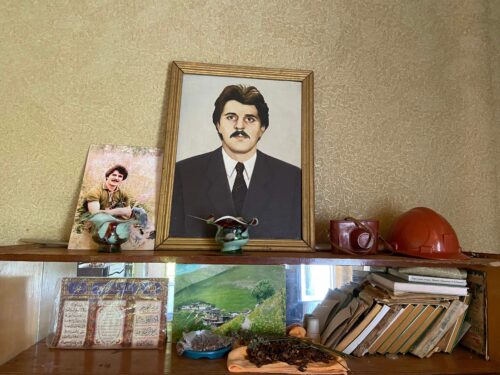
After getting approval from Sitka Tribe of Alaska’s Tribal Council, I recently spent a year conducting dissertation fieldwork among Tlingit people in Sheet’ká (Sitka). Through our conversations, I learned how over 200 years of government-sanctioned medicalized and racialized abuses made many people initially hesitant to get vaccinated against COVID-19.
Few stories embody these injustices better than an experiment to test the efficacy of the vaccine for tuberculosis, Bacille Calmette-Guérin (BCG)—a vaccine that, coincidentally, is now showing promise in helping people with Type 1 diabetes avoid severe disease from COVID-19.
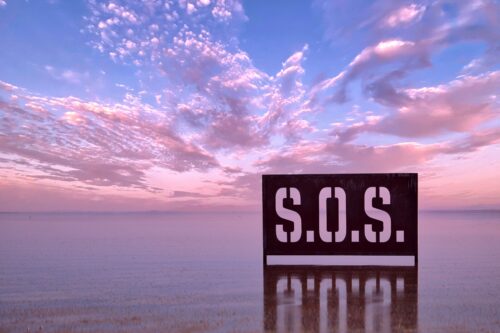
Beginning in the 1940s, the Territory of Alaska faced an epidemic of TB, with mortality rates eight times that of the U.S by the 1950s. Decades of governmental neglect had left many Alaska Native communities, in particular, without adequate health care and infrastructure. Mortality rates from TB in these communities were close to 30 times that of White people. A 1954 federal health report acknowledged the lack of health care, noting “neither the Federal nor Territorial Governments had provided more than a modicum of care for the tuberculosis” for Alaska Natives.
This sustained rate of TB—and concerns that the epidemic could further spread outside of Alaska Native communities to predominantly White populations in Alaska—prompted health officials to consider using the BCG vaccine. However, at that point, the vaccine’s efficacy was unproven.
So, two physicians—Dr. Joseph Aronson and Dr. Carroll Palmer—got support from the Office of Indian Affairs and the U.S. Public Health Service to test the efficacy of the BCG vaccine. These doctors enrolled nearly 3,000 Indigenous people across the U.S. in the study. The researchers targeted Indigenous villages where “economic conditions in all areas were uniformly poor, housing was poor and crowded, and morbidity and mortality from tuberculosis were reported as being high,” particularly in Southeast Alaska. But instead of these villages being sites for public health intervention, they became sites for experimentation.
There was no documented consent procedure from the Indigenous people in this study, most of whom were under the age of 18. In an article published later, the doctors noted they conducted the experiment at “reservations,” a general term they used to denote “reservations, tribes, schools, or geographic region.” Most likely, the doctors used students at Alaska Native boarding schools as a test population for their experiments.
Protecting Alaska Native lives—particularly those who researchers identified as vulnerable—seemed to mean little to the state’s public health institutions. The doctors apparently saw potential deaths from this experiment, whether they were in the test or control group, as acceptable. They seemed to have wrongfully believed that the ends justified the means.
Ultimately, the vaccine was found to be successful at preventing TB. Yet, even after using Indigenous children as test subjects, government officials did not widely distribute the vaccine to Alaska Native populations. In fact, they only administered the vaccine to about 2,000 to 3,000 Alaska Natives, or less than 2 percent of the territory’s total population, primarily between 1949 and 1953. They defended this decision in part by saying the vaccine was “not completely or 100 percent protective”—a statement that could be made of any vaccine.
The bottom line: The government and public health experts apparently saw Alaska Natives’ lives as valuable primarily when their bodies could be used to test the efficacy of a vaccine—not as people who deserved to receive the potentially lifesaving results of that biomedical research.
Events such as this likely feel painfully familiar for those who are aware of other medical injustices in the U.S.
Take, for example, the case of Henrietta Lacks, a Black woman whose cells were used by medical researchers without her consent and without financial compensation in the 1950s. Her White doctors used the cells to create some of the most valuable medical advances of the time, even as Lacks’ family struggled to make ends meet.
And like the BCG experiment, in the 1960s and 1970s, physicians tested treatments for trachoma on Indigenous children—but their parents had not given consent. These are but two events in an extensive list that includes doctors’ use of enslaved Black bodies for experiments, the use of stolen Black bodies as medical school cadavers, and the forced sterilization of Indigenous, Black, and Puerto Rican women.
Read more from the archives: “Why Are Black People’s Remains in Museums?”
While doing research in Sheet’ká from 2020 to 2021, I found that many Tlingit interlocutors were aware of injustices like these. Nearly every Tlingit person I spoke with either knew or knew of someone who had endured nonconsensual medical procedures. And those who didn’t know anyone directly affected grew up hearing stories—fiercely debated among historians—about the U.S. government sending blankets infected with smallpox to Indigenous communities as a form of biological warfare.
When I asked people about their initial attitudes toward COVID-19 vaccines, many told me they didn’t feel like they could trust public health institutions and the government because of these histories. They felt uncomfortable having to place their trust in institutions that had brought their communities so much harm.
Despite this, many in health care and various media outlets often paint vaccine hesitancy as a problem of education: If only people “knew better,” then they would get vaccinated. But the truth is, the Tlingit people I spoke with knew much more about the history of medical ethics in the U.S. than most of the White people I spoke with in Sheet’ká.
The Urban Indian Health Institute and similar organizations that prioritize listening to Native communities have successfully addressed vaccine hesitancy by working with elders and centering local values. In Sheet’ká, the Sitka Tribe of Alaska asked Tribal Council members to share why many of them ultimately chose to get vaccinated and why they felt others should do the same. Their messages focused on the importance of protecting the most vulnerable in their communities from the harms of COVID-19.
In the end, despite ongoing settler colonial violence and painful memories, most Tlingit people I spoke with got COVID-19 vaccines. Their love, compassion, and care for their community and its past have led them since time immemorial and continue to do so today—a lesson that all public health officials should take to heart.