Death as Something We Make

Renee (a pseudonym) closed her eyes, lay her head in her brother’s arms, and gently drew her last breath. Minutes before, she had chugged a bitter concoction of Seconal and juice, while the loved ones encircling her offered their final blessings and softly sang her out of this world.
This carefully choreographed scene was exactly the way Renee had imagined her death after months of careful planning. She had endured a grueling course of cancer treatments several years prior. When the cancer recurred and metastasized, she was quickly drawn to the possibility of a medically assisted death. As a resident of Vermont, she became one of the roughly 1 in 5 Americans legally permitted to end their lives when faced with a terminal illness.
Medical aid-in-dying (MAID), currently legal in 10 U.S. jurisdictions, with another poised to likely follow soon, authorizes physicians to prescribe a lethal dose of medication to a terminally ill, mentally competent adult patient. With legislative safeguards in place to protect against abuse, and many physicians reluctant to participate, the process is neither easy nor guaranteed. But the very prospect of MAID is changing the way people in the U.S. and elsewhere in the world think about death.
As the pandemic has made avoiding the subject of death all but impossible, planning for death has taken on new urgency. Palliative care experts have urged people to document end-of-life wishes in advance directives, while end-of-life startups have tapped into the market potential of death. These developments align with what has long been a strong motivation for terminally ill people seeking MAID: to control and carefully craft the scene of death.
I am a medical anthropologist who has spent the past five years studying the implementation of Vermont’s 2013 Patient Choice and Control at End of Life Act. I interviewed over 140 patients, health care providers, caregivers, activists, and legislators to collect their stories and experiences. I also attended medical conferences and advocacy events where MAID was being discussed.
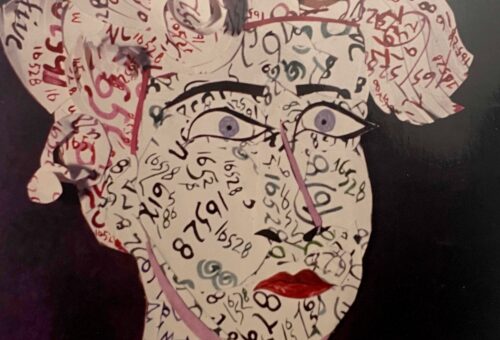
While I learned a lot about what drives people to MAID, I was particularly fascinated by what MAID does to death. The option transforms death from an object of dread to an anticipated occasion that may be painstakingly planned, staged, and produced. The theatrical imagery is intentional: An assisted death is an event that one scripts, a matter of careful timing, with a well-designed set and the right supporting cast. Through this process, death becomes not just something that happens but also something that is made.
The four friends I interviewed about Renee’s life and death all used similar words to describe her: independent, stubborn, strong-willed, even a bit of a curmudgeon. She loved being a crone, what some people define as a woman who has gone through menopause and stands in her power and wisdom. She never married nor had a significant romantic relationship, which was a source of sorrow for her. Still, her life was rich with friendships, meaningful work as an artist and teacher, and a devoted spiritual practice.
Renee was also dignified. A friend recounted how, during a spiritual retreat, a group was doing a silent meditation while walking outdoors. They stumbled upon Renee, up to her breasts in snow, waving calmly.
“She had fallen through a spot and was literally stuck in the snow up to her chest, but she was just like, ‘Um, excuse me,’” her friend recounted. “Where other people might be thrashing around or screaming for help, she was just like, ‘Hello.’ And that’s a really good way of describing her.”
As her cancer progressed, Renee was in constant pain. She rejected strong pain medications to avoid a foggy brain. Fluid built up in her chest, affecting her breathing. An intensely private and independent person, she did not want to depend on others for care at the end of life. And she did not want to be stuck in her body longer than it could be useful to her.
Renee loved her life, but she knew where her illness was headed. When she reached the limits of what she thought she could bear, MAID offered an enticing pathway out.
Historically, humans have largely been passive witnesses to their own deaths. Since the middle of the 20th century, however, technological developments in medicine have offered increasing possibilities for human control over one’s own death. These changes have led to heated debates about what counts as death and altered the kind of event we take death to be.
MAID renders not only the time of death but also the broader landscape of death open to human control. MAID allows terminally ill patients to choreograph their own deaths, deciding not only when but where and how and with whom. Part of the appeal is that one must go on living right up until the moment of death. It takes work to engage in all the planning; it keeps one vibrant and busy. There are people to call, papers to file, and scenes to set. Making death turns dying into an active extension of life.
Staging death in this way also allows the dying person to sidestep the messiness of death—the bodily fluids and decay—what the sociologist Julia Lawton has called the “dirtiness” of death. MAID makes it possible to attempt a calm, orderly, sanitized death. Some deliberately empty their bladder or bowels in advance, or plan to wear diapers. A “good death,” from this perspective, has not only an ethical but also an aesthetic quality.
Of course, this sort of staging is not without controversy. For some, it represents unwelcome interference with God’s plans. For people like Renee, however, it infuses one’s death with personal meaning and control.
Renee set the weekend for her death to avoid another hospitalization to drain fluid from her chest, a procedure she had undergone several times. Determined not to face hospitalization again, she bought a plane ticket for a spiritual mentor who lived in another state and invited a small group of family and friends to gather at her home.
It was an emotional but humor-filled weekend. “She didn’t want us to be all sad and heavy about it. She wanted to have a good time,” one friend recalled.
Her friends were amused by the incongruously frenetic pace of her dying. All weekend, Renee shuffled around the house, shredding papers and making lists and phone calls. Her friends made up a playful song, “Follow the Little Blue Hose,” set to the tune of “Follow the Yellow Brick Road” from the film The Wizard of Oz, which they sang as they watched her scurry around trailed by an oxygen tank.
Medical aid-in-dying transforms death from an object of dread to an anticipated occasion that may be planned, staged, and produced.
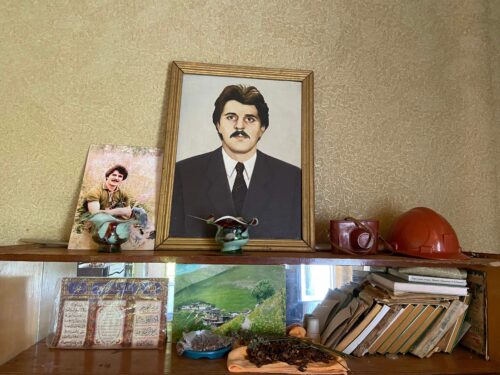
Renee was very organized about dying. She had thought about which people she wanted to inherit her dog, her journals, and her art. She ordered dry ice for her in-home wake and wrote a check to the crematorium and clipped it to the relevant paperwork. She even finished her taxes. She left detailed instructions for her postmortem care and funeral in a file to be opened after her death. A pine casket, constructed by a friend, had been sitting in her shed for months. The only matter left to attend to was her actual death.
Renee had never been certain she would take the lethal dose of Seconal. (In Oregon, only about 64 percent of people who obtain the medication go on to ingest it.) Initially, she hoped she might avoid it by willing herself to die. A natural death was more aligned with her worldview and spiritual practice. Her friends performed an “unbinding” ceremony in an effort to untether her soul from her body.
But she couldn’t make herself go. And if she didn’t die, her friends would need to go home, and she would be expected at the hospital on Tuesday, which had become, for her, a fate worse than death.
When Renee went to bed Saturday night, she had not yet made up her mind about what she would do. During the night, her intense coughing echoed throughout the house. Finally, she got up at 4 a.m., grabbed her laptop, and went back to her bedroom to pen love letters to friends. At 6 a.m., she emerged and announced she was ready to go.
While Renee said her goodbyes, four friends sat in a circle and prepared the medication with a makeshift ritual ceremony. Using beautiful pottery and sacred chalices, they emptied 100 capsules—the number of Seconal pills required to form a lethal dose—singing while they worked, and carefully mixed the powder with juice. They all piled on the couch for a final photo shoot. Renee laid across their laps in a favorite leopard print and purple velvet outfit.
Then, in her signature no-nonsense style, Renee got into bed and started directing everyone on where to stand. They surrounded her as she drank, chanting softly. Ten minutes later, she was dead.
Some health care providers I’ve talked to worry over the portrayal of deaths like Renee’s. There is a danger in suggesting that death should be clean and orderly, they rightfully suggest, when most deaths are far from it. Media accounts of glamorized assisted deaths may set up unrealistic expectations for what death should look like.
And some MAID deaths fail to follow the plan, as I learned from my research. There was the woman who took hours and hours to die, scaring her children when she repeatedly turned blue, then miraculously started breathing again. There was also the man who swallowed a dose of morphine that “should have killed a grizzly bear,” according to his physician, yet who nevertheless awoke the next morning.
In my experience, however, most of the bereaved remain deeply satisfied with their loved one’s medically assisted death. They tend to view supporting a loved one’s wishes for MAID as an ultimate form of care and being by their side as a consummate honor.
After she died, Renee’s friends quickly got to work implementing her plans. They called the hospice nurse to pronounce her dead. They notified people, following a list Renee had annotated with her characteristic wit: those to be nice to, those she really didn’t give a shit about but should probably know that she had died. Three women washed and anointed her body with meticulous care. The coffin was set up in the living room for a three-day in-home wake. Renee’s funeral was held in the same room, then a friend drove her body to the crematorium, followed by a caravan of other friends.
Hilarity frequently punctured the somber mood. “It was just like a comedy of errors,” a friend recalled. “The dry ice all melted, like a day or three days earlier than it should have, the casket almost didn’t fit in the car. … Right until the last minute, we were like, ‘Thanks, Renee,’ you know, like, ‘good planning on that one.’”
Despite these hiccups, the friends who participated in Renee’s death felt extraordinarily honored to be present. They saw her final act as brave and dignified, very much aligned with the way she lived her life. “It takes personality, at least that’s my impression,” one friend said. “It’s hugely courageous to go, ‘All right, in this minute, I’m gonna be here, and the next minute, I’m not. Here I go to make that happen. I’m gonna make that happen right now.’”
This comment captures an important feature of MAID: For observers, there is something startling about going from being fully alive one minute, and then, suddenly, willfully dead. Aside from suicide, this is not how we’re taught our own deaths happen.
But MAID is shifting the stakes of what we think death might be—transforming death into something we make.