Living With the Prospect of Assisted Dying

Excerpted from The Day I Die: The Untold Story of Assisted Dying in America by Anita Hannig. © 2022 by Anita Hannig. Used with permission of the publisher, Sourcebooks, Inc. All rights reserved.
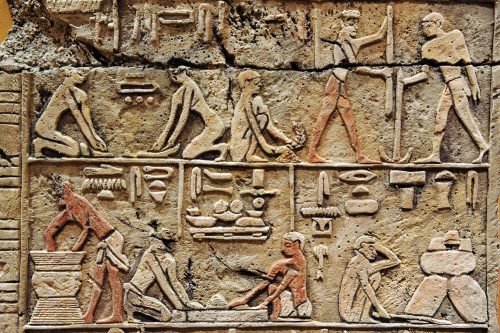
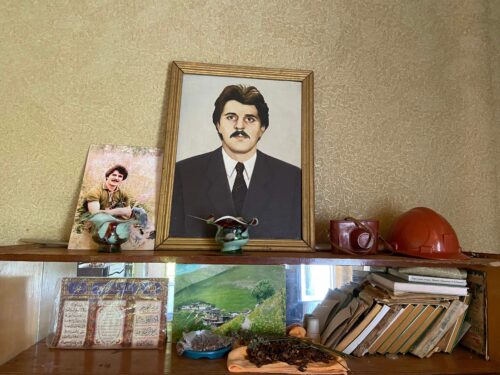
Covering the walls in Joe’s home office in Vancouver, Washington, were dozens of glossy medals and framed pictures of running meets—a shrine to the hours and days he had spent pushing himself to the crest of physical triumph. [1] [1] All names of interviewees have been changed to protect people’s privacy. Each of them carried vivid memories of carbo-loading dinners, auspicious bib numbers, and sports drinks in all colors of the rainbow. Now they served as blunt reminders of the life he once had, prediagnosis, when the muscles in his body still stretched, lunged, and churned without special effort, or even thought.
One of the photos shows Joe, probably in his late forties, in dark-blue shorts and a bright-yellow T-shirt. His short hair hemmed in by a white headband, he wears aviator sunglasses and a look of concentration on his face as he sprints the last couple of miles toward the finish line of the Portland marathon. The course flattens out here as runners weave their way through the downtown area to a shrill chorus of bystanders. Right behind Joe, a younger man with wiry legs picks up the chase. But Joe stares straight ahead, and his stride looks strong. It’s clear that he won’t go down without a fight.
By the time I met Joe on a Sunday morning in early 2018, the days of his physical feats were long gone. As I walked up to greet him, he lay immobile in the middle of his living room in a dark leather recliner. A brown duvet was pulled up to his neck, warming a body that wouldn’t obey him anymore. Solemn and alert, Joe’s denim-blue eyes peered out at me from behind his round, metal-rimmed glasses. Behind him, the rain drummed on a sliding glass door that opened into a drenched backyard. The rain wasn’t unusual for this time of year, late February in the Pacific Northwest, but it added a brittle layer of gloom to the space.
When I had called his partner, Anna, to arrange the visit, she immediately launched into a description of all the roadblocks she and Joe had been facing to qualify him for Washington’s assisted dying law. She was talking fast, like a person frustrated by an unmet desire to be heard. I knew from my research with other families that navigating the bureaucracy of assisted dying laws could be a full-time job. But I was surprised to learn that someone with a clear-cut terminal diagnosis was having such difficulty.
In September 2016, at age 72, Joe was diagnosed with ALS—amyotrophic lateral sclerosis, also known as Lou Gehrig’s disease—a progressive neurological disorder that destroys neurons responsible for muscle movement. In the United States, about 6,000 people are diagnosed with ALS every year, and the disease’s etiology still remains largely a mystery. After the initial onset of symptoms, the average life expectancy ranges from two to five years as the body’s muscle groups shut down one by one.
Joe was polite and soft-spoken. His lopsided smile, encased by a closely trimmed snow-white beard, surfaced only occasionally, when something truly amused him. Half an hour into our conversation, as I asked Joe and Anna to reconstruct the events of the past year and a half, Joe broke into a metallic cough. He motioned his chin toward the glass of water that sat between him and Anna on a side table.
“His mouth has felt exceptionally dry today,” Anna offered by way of an explanation. She picked up the glass and held it for him, waiting for his tongue to catch the straw.
“I think I may have to have a manual cough assist,” Joe whispered, his voice grainy and barely audible. Anna rose to her feet.
“With ALS, you lose your core strength, your diaphragm, which you need for coughing,” Anna said as she peeled the duvet from Joe’s body, baring his pale arms and legs, which had lost nearly all muscle definition. “So we have a machine to clear the mucus in his airway, but Joe has discovered that this little thing we do is actually more effective.”
Anna removed his head and neck rests and pressed a button on his recliner. Joe’s body slid slowly down and out of the chair. When his furry moccasin slippers hit the ground, she hoisted him up—he could still stand, but his upper body was so limp that he almost toppled over—and scooped him up from behind. Though Anna was much smaller than Joe, she didn’t seem to be straining. Joe was thin as a wafer.
Read more on medical aid-in-dying, from the archives: “Death as Something We Make”
Joe hung in Anna’s arms like a rag doll—his head drooping low on his chest, shoulders perched forward, and arms sagging by his sides like two power lines cut down by a storm. He used to be a tall man, but the disease had compressed his spinal cord.
Anna tightened her embrace and folded her hands flat on top of each other underneath his rib cage. “Ready?” she asked.
Joe murmured his response, looking straight down. On the count of three, Anna dug her hands into his abdomen in a quick upward motion while Joe tried to clear his throat. A feeble sound emerged. She pressed in again. Again.
“It takes timing, but, you know, we’re dancers. We’ve got timing,” she said, shooting me an apologetic glance. I told her that I didn’t mind, wishing she could forget about me for a second, a witness to their tragic dance.
The fourth time, Joe emitted a forceful, guttural cough. “That was a good one,” Anna said, carefully releasing her embrace and helping Joe sink back into his recliner. He was still looking down, his neck muscles no longer strong enough to keep his head upright.
“You can see this is just a laugh a minute, isn’t it?” Anna said, trying to diffuse the lingering intimacy between us. She tucked her straight, silver hair behind her ears and stole a quick glance at Joe. He cracked a smile, fleeting but just in time for her to catch it.
Anna settled Joe back into the chair, propping his head up with two pillows and his neck brace. She knew exactly how to arrange everything. You could tell she had done it a hundred times. The whole ordeal had made Joe thirsty, and he had her lift the glass of water to his lips again so he could bite down on the straw. Joe closed his eyes. For a second, I wondered if he was going to drift off to sleep, but then he opened them again and looked at me, ready for the next question.
In the midsummer of 2016, Joe noticed weakness in his left hand during his weekly pickleball game. Pickleball combines elements of badminton, tennis, and table tennis. Players wield wooden or composite paddles on a small court. Joe was right-handed, but he couldn’t get a good grip anymore when he used his left hand to pick up the ball. Maybe a pinched nerve, he speculated. But when the sensation didn’t go away weeks later, he went to see a neurologist.
Anna was standing in the kitchen when Joe returned from his appointment. She had no reason to feel alarmed. She thought he was going to tell her that they had scheduled an MRI or X-ray for him. But he had other news for her.
“Everybody has to die some time,” Joe said.
“What?” Anna felt the ground turn unsteady beneath her feet.
“The doctor is pretty sure, in fact, he’s certain, that I have ALS.” Joe understood that ALS was fatal, but he didn’t have any idea of how the disease would progress. His neurologist hadn’t gone into much detail with him that day.
Anna clutched the counter and burst into tears. She knew exactly what an ALS diagnosis meant. One of her elementary school friends, a dentist, had died of ALS in his late thirties. She knew that ALS led to paralysis and went from one part of the body to another while the brain remained completely active—“a cruel joke,” she called it.
“Everybody has to die some time,” Joe said.
Tom Samuels, one of the pulmonology specialists Joe started seeing months later, had long studied the unique challenges an ALS diagnosis brings. When I met Samuels at a coffee shop in Portland, he explained that ALS impacts three different groups of muscles.
“ALS affects the extremities, so arms and legs,” he said. “In about two-thirds of patients, that’s the first thing they notice. They may get a little foot drop or weakness in one hand that progresses. About a third of all patients, the first thing that goes is their speech and the ability to swallow. It’s called bulbar onset. Then, about one percent of patients, the first thing they notice is shortness of breath, because the breathing muscles become affected.”
“But everyone eventually gets everything,” he added. “If they live long enough.”
I asked Samuels what patients with ALS eventually die from.
“Ninety-nine percent die from respiratory failure,” he said. “The breathing muscles get so weak that they can’t get carbon dioxide out. So the carbon dioxide builds up. The good news about that is that carbon dioxide acts like morphine on the brain—it basically puts the brain to sleep. It’s usually not a sudden episode; they usually have a buildup, lapse into a coma, and then they die. But occasionally people will choke to death. It’s a miserable way to die.”
Samuels’s explanation made me see Anna’s Heimlich maneuver in a new light. Had Joe been terrified of choking to death the morning I met him? If most patients with ALS could expect a death from respiratory failure, as Samuels suggested they did, then running out the clock on an ALS diagnosis didn’t seem like an especially comforting option.
In a society that trades in military metaphors when talking about illness—when cancer patients become “warriors” and “survivors” and cells foreign “invaders”—the idea of foregoing even the sliver of a chance for more time can feel like premature surrender. After all, the next miracle cure could be just around the corner, the next experimental drug one clinical trial away.
“Abuse of the military metaphor may be inevitable in a capitalist society,” wrote philosopher and writer Susan Sontag. “War-making is one of the few activities that people are not supposed to view ‘realistically,’ that is, with an eye to expense and practical outcome. In all-out war, expenditure is all-out, unprudent—war being defined as an emergency in which no sacrifice is excessive.”
The idea of foregoing even the sliver of a chance for more time can feel like premature surrender.
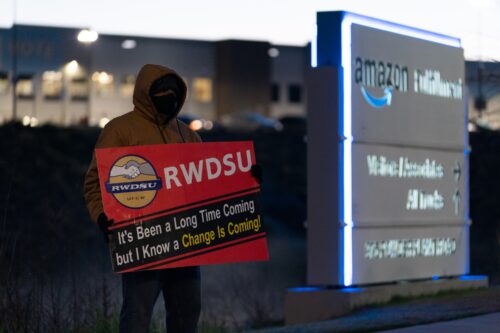
Turning your back on the powerful cultural machinery of life extension can feel like trying to swim upstream. That’s why some assisted dying patients struggle with being perceived as “quitters” when they push back against the ubiquitous logic that more time is always better. The decision to stop “fighting” to reclaim what life someone is able to have here and now almost amounts to an act of conscientious objection.
For his part, Joe had no intention of running the full gamut of what ALS held in store for him: the air hunger that would only get worse and the prospect of becoming “locked in”—when he would no longer be able to move or speak or swallow but would remain mentally alert. Joe’s initial frustration over not having any viable treatment options soon gave way to a decision. He wouldn’t let this brutal disease get the best of him, only waiting for the other shoe to drop—not if he could help it. He would be the one to decide when and how he was going to die.
He would hasten the end of his life.
This excerpt has been lightly edited for style, length, and clarity.