U.S. Coronavirus Advice Is Failing Pregnant Women

As much as it feels like day-to-day life has been suspended in the time of the COVID-19 pandemic, one thing cannot be put on pause: childbirth. On average, more than 10,000 babies are born every day in the United States.
In response to the COVID-19 crisis, the U.S. Centers for Disease Control and Prevention (CDC) and the American College of Obstetricians and Gynecologists (ACOG) released guidelines stating that health care facilities, on a case-by-case basis, may consider separating women with suspected or confirmed COVID-19 from their newborns until there is no longer a concern for transmission.
These recommendations are substantially more cautious than advice from the World Health Organization (WHO), which does not mention any form of separation but instead emphasizes the importance of early breastfeeding, skin-to-skin contact, and room-sharing with newborns for mothers infected with COVID-19. New breastfeeding guidelines from WHO specifically say not to separate mother and baby when a mother is well enough to breastfeed, even in cases of confirmed or suspected COVID-19.
Unfortunately, the U.S. maternity care response to the COVID-19 crisis is not really so surprising: It is emblematic of the standard—and misguided—“better safe than sorry” policies in the United States for maternity care.
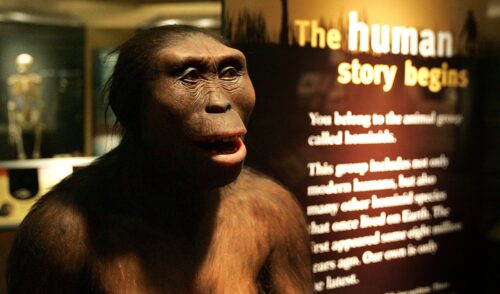
As a biological anthropologist who has studied the intergenerational effects of maternal stress for the last 12 years, it is clear to me that U.S. policies treat childbirth as a sickness rather than as a natural process shaped by millions of years of cultural and biological evolution.
While hospitals and modern medicine save the lives of women and newborns who face serious medical complications, the fact is that most pregnancies are low risk and do not involve such difficulties. The health care environment in the United States, however, is set up so that most pregnant women are funneled into receiving the same medicalized care, regardless of risk.
The result is shockingly high rates of medical intervention in the U.S. for women giving birth: Cesarean section, for example, increased by 53 percent from 1996 to 2007. The current rate of 32 percent is more than twice what WHO estimates as the percent likely to be medically necessary. Other types of interventions that many say are overused include restrictions on eating and drinking in labor, the use of continuous electronic fetal monitoring, speeding up labor through drug administration, and episiotomies.
Critics say the overuse of these interventions not only causes the United States to spend more on maternity care than any other country in the world, but that it also results in physical and emotional costs to women.
Despite the high costs of the U.S. medical system, the country experiences the highest rate of maternal mortality among a set of 10 similarly high-income countries. For every 100,000 live births, 14 American women die during pregnancy, at birth, or within about a month of childbirth—that’s significantly more than in the United Kingdom, where 9 women die for every 100,000 babies.
All of these problems have been amplified and highlighted as the coronavirus sweeps through the United States. I am currently co-leading a study with Dartmouth College biological anthropologist Theresa Gildner that evaluates the impacts of the COVID-19 pandemic on pregnant women’s well-being and health care experiences. Our preliminary results throw a spotlight on these issues.
There are several core problems with the current advice in the U.S. on birthing during the pandemic.
For one, the CDC recommends that the “costs and benefits” of separating mothers from their newborns should be discussed with the pregnant mother—with women being left to make the decision. However, in our study, women reported being unclear about whether or not they are allowed to actually refuse separation from their child after it is born. Even before the pandemic, many women—and in particular women of color—often reported feeling disempowered about their birthing experience. The CDC’s recommendations could make this situation worse.
The potential benefit of separating infants is that it may reduce their risk of contracting COVID-19. Some newborns have tested positive for COVID-19 and even, tragically, died. But the risks and the impacts of COVID-19 for all infants, including those without preexisting medical conditions, remain unclear.
The cons associated with maternal-newborn separation, however, are very clear. Experts consider immediate skin-to-skin contact essential for helping newborns regulate their body temperature after birth, and it’s associated with lower mortality. Mothers who are able to immediately practice skin-to-skin contact breastfeed their infants longer, which is important since breast milk is known to be good for an infant’s immune system. So, it could be helpful for newborns who might be exposed to infection.
At the height of the pandemic along the East Coast, some hospitals forced women to labor alone.
Mother and newborn separation can also hurt maternal emotional well-being, contributing to postpartum depression and even post-traumatic stress disorder. For example, in one 2019 pre-pandemic study, mothers of very premature infants cared for in single-family rooms (as opposed to an open bay unit, a form of separation) had significantly lower depression scores. Both mothers and fathers of the single-family room infants reported less stress during hospitalization.
Maternal contact—including smell, touch, and voice—can impact a child’s physiological responses to stress and, potentially, their later health. One study reported that 2-day-old newborns who slept alone had a 176 percent increase in their stress response relative to newborns who were sleeping in skin-to-skin contact with their mothers.
It is hard to weigh the medical pros and cons, and as an anthropologist, it is not my job to say what the right approach is. But it is clear that the U.S. recommendations are more cautious than WHO’s, emphasizing possible harms over benefits when it comes to mothers who tested positive for or are suspected of having COVID-19 staying with their newborns.
Notably, the CDC has also recommended that health care facilities consider limiting to one the number of support persons available to women in labor—forcing her to choose between a partner, parent, sibling, friend, or doula. At the height of the pandemic along the East Coast, some hospitals forced women to labor alone. Among women who have participated in our COVID-19 study, many have described being told that they will have to deliver via cesarean without loved ones in the room or that they will need to labor alone if they are COVID-19 positive.
Eliminating support teams comes with costs. Evidence shows that having continuous support throughout labor improves both maternal and newborn outcomes, including a better chance of women having a vaginal delivery (as opposed to a caesarian section), fewer interventions with instruments like a vacuum and forceps, and better newborn health.
Trained support people, such as doulas, are particularly helpful because they serve as both emotional support and advocates for women during delivery. Not counting doulas as essential staff could disproportionately affect women of color, who are already more likely to be treated poorly by hospital staff.
Media stories have reported that fears surrounding COVID-19 have led to an increased interest in alternatives to hospital birth—from home birth to birthing centers, often with the attendance of a midwife.
Those kinds of births aren’t common in the United States: Only 10 percent of births are attended by midwives, with 1.6 percent of women giving birth at home (usually with midwives). In contrast, in New Zealand, midwives are the lead maternity caregivers for almost 92 percent of pregnancies, and 4 percent of births occur at home.
Evidence suggests that for women with uncomplicated pregnancies, the chance of having an intervention-free birth is higher when women deliver with a midwife in a birthing center or at home than in the hospital. The U.K.’s National Health Service and the Ministry of Health in New Zealand explain that home birth can be a reasonable option for women who are low-risk. In contrast, ACOG guidelines state that hospitals and accredited birth centers are the “safest” setting for birth.
Unfortunately, structural factors have long prohibited access to non-hospital care for many U.S. women. Private insurance companies often do not reimburse for home births, and Medicaid, which pays for just under half of all births, only covers home birth in approximately half of the states. Women who decide to give birth in their home may have to pay for that out of pocket. In our COVID-19 study, many participants stated that despite a preference for home birth, they were unable to follow their wishes due to cost or because they perceived home births to be illegal in their state.
Stand-alone birthing centers, which only cater to laboring mothers and provide more home-like settings, could also be attractive options for individuals seeking an alternative to hospital-based maternity care. A large study of 46,000 Medicaid recipients found that among women with similar risks, those who received care at birth centers were less likely to have babies born preterm, less likely to have a cesarean, and twice as likely to have a vaginal birth after having had a cesarean. What’s more, the cost for care for women going to birth centers was nearly US$2,000 less than average. Stand-alone birthing centers have been rapidly popping up over the last 10 years, but there are still fewer than 400 in the entire United States; some states have none.
Part of the reason for this is that certified nurse midwives are not independent practitioners in all states, meaning that midwives need to work with or under a physician if they want to open a birthing center. Some Certificate of Need laws state that hospitals (which would be competitors of such birth centers) need to support centers opening.
The result is that access to free-standing birthing centers, and midwifery care more generally, is alarmingly limited in the United States.
The coronavirus pandemic has raised public awareness about the conditions many U.S. women are forced into while giving birth.
The general approach to maternal and newborn care in the United States is not based on understanding individual women’s preferences and risk. Instead, it has arisen from the unfounded assumption that more technology, medicine, and intervention in childbirth is “safer.”
There are some immediate and practical steps that should be taken to improve things during the pandemic: for example, getting pregnant women out of hospitals and into dedicated birth centers, enacting policy changes to ensure that insurance covers home births, and allowing all qualified midwives to act as independent practitioners in every state. In addition, doulas without symptoms or those who test negative for COVID-19 should also be considered as part of a pregnant woman’s care team, not counting as the one allowable companion for a laboring mother. On a promising note, the governor of New York launched a state task force to determine how to authorize additional birthing centers that women could go to instead of hospitals.
In the longer term, increasing and standardizing Medicaid and private-insurance reimbursement rates for midwife-attended births, and exempting birth centers from Certificate of Need laws, would help boost access to out-of-hospital birthing spaces. For many women, hospitals will remain their choice of place for birth, and that’s fine—but it’s important for U.S. women to be aware of the potential benefits of alternatives and to have access to those alternatives if they choose them.
On the other side of the COVID-19 crisis, some of the pressure on the U.S. medical system will be relieved. Now is the time to think about common health care practices associated with birth in the United States and to question their continued utility and humaneness.