When Doctors Don’t Listen
It’s been almost a year since I tried to kill myself.
As a doctoral student living in the leafy suburb of Brookline, Massachusetts, in 2015, I chanced upon a tick—a tiny vampire the size of a poppy seed—that changed my life forever and nearly brought it to an end.
After being bitten by the tick, I was plagued with full-body joint pain, muscle twitching, night-time seizures, cardiac abnormalities, depression, fatigue, and other neurological disturbances. Early on, this confluence of symptoms confounded doctors. Upon hearing my account, one neurologist shook his head. “That doesn’t make any sense,” he said, before suggesting that my caffeine intake might be responsible. I was told repeatedly by various doctors that the mysterious ailment darkening my existence was psychological in nature, most likely due to stress. It took 12 months before I was finally diagnosed with Lyme disease. But little changed after the diagnosis, contrary to what I had naively expected. My doctor prescribed four weeks of antibiotics and told me that if the medication didn’t work then it wasn’t Lyme. The antibiotics didn’t work.
Suddenly, I was alone—exiled from my body and others. My disease has been exacerbated by the social consequences of having a complex chronic condition. When an illness isn’t medically recognized or refuses to progress in a straightforward way toward better health, those around you often grow impatient or suspicious. People stop asking how you are or act as if your failure to recover is somehow a personal weakness. These silences and reactions can drive the chronically ill into isolation, despair, and existential confusion.
Sufferers are also often alienated by the unhealthy dynamics that characterize many doctor-patient interactions in the Western world today. The power imbalance between who can authoritatively describe what is going on in the body and who can’t has a deep impact on how illness is experienced and navigated. Doctors hold the authority to determine which bits of a patient’s story are useful, which interpretations to act on, and which diagnostic tests are made available. The doctors and specialists I consulted consistently interrupted me, refused to order tests, and denied the severity of my symptoms. The subtle and oftentimes brutal rejection of my experiential knowledge and suffering slowly anesthetized me against hope.
I can see why this happens. Doctors face time and financial constraints, heavy workloads, and distrusting and contentious patients. They are taught to prioritize their technical capabilities and are faced with the challenging task of combing through irrelevant information for what is medically relevant. As a way to cope with a daily barrage of problems and complaints—and the deaths of some of their patients—some physicians become callous and numb.
The practice of medicine in the 21st century is a complex affair. But even under such conditions, appreciating the singularity of an individual’s life is essential to providing authentic care and good medicine. As the late neurologist and author Oliver Sacks wrote, practical scientific medicine and existential medicine are separate but inseparable—“not contradictory but complementary.”
Paternalistic relationships between doctors and patients in today’s medical system cause harm to many individuals. For me, they delayed my diagnosis, protracted my illness, denied me a sense of being validated and understood, and conspired to push me deeper into the depths of my despair. The practice of modern medicine doesn’t have to be this way.
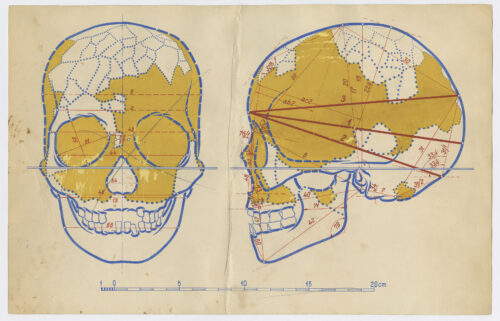
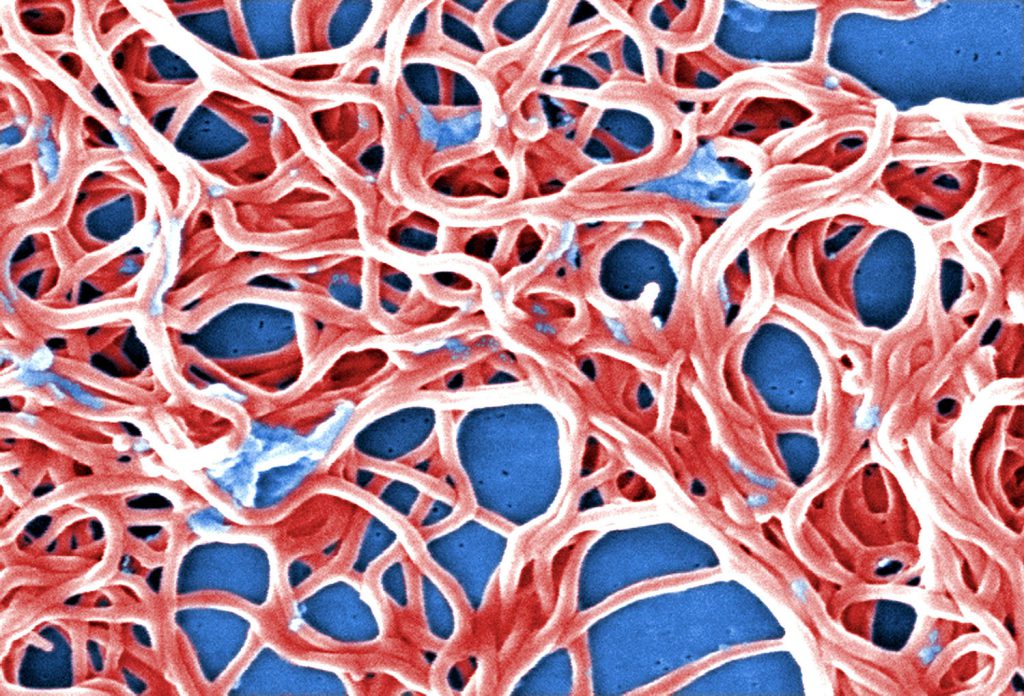
The bacterium responsible for Lyme disease has a long history in North America. Katharine Walter, who studies infectious diseases at Stanford University, and her team recently collected and sequenced 148 genomes of the microorganism and found that it has cycled through forests for at least 60,000 years. But it was only as recently as 1982 that medical entomologist Willy Burgdorfer identified the tiny corkscrew-shaped bacterium mysteriously afflicting some residents of Lyme, Old Lyme, and East Haddam, Connecticut, and Long Island, New York. In recognition of the discovery, the bacterial pathogen was christened in his name: Borrelia burgdorferi.
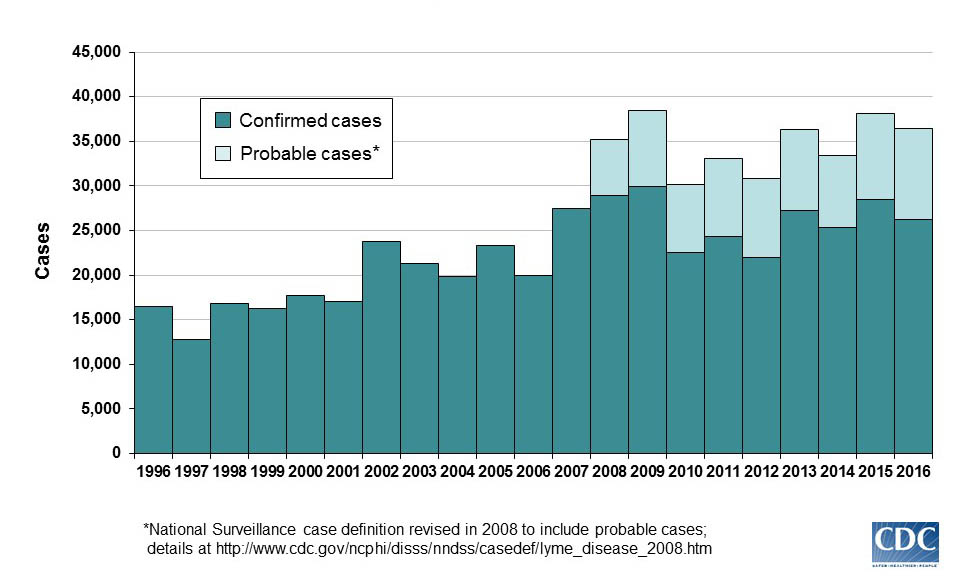
The Centers for Disease Control and Prevention (CDC) receives reports of approximately 30,000 cases of Lyme disease annually in the United States. However, the organization estimates that about 300,000 people contract the illness each year. A variety of factors contribute to this significant disparity—but a dearth of reliable diagnostic tests is a key part of the problem.
The CDC recommends a two-tiered blood test to spot antibodies against the B. burgdorferi bacteria. But this test is notoriously unreliable, in part because it was developed to track a group of Lyme patients, rather than for clinical diagnosis. Yet this inadequate test became the national standard for both doctors and insurance companies. As a result, there are many patients whose tests come back negative even though they are positive for Lyme disease.
After overcoming the first hurdle of diagnosis, most patients face a treatment protocol that is also controversial. According to the Infectious Diseases Society of America (IDSA), a course of up to 28 days of antibiotics is recommended for those diagnosed with Lyme. Yet according to the International Lyme and Associated Diseases Society, a short course of antibiotics is often insufficient for treating Lyme. And some clinicians have found that longer treatments benefit patients.
While the IDSA does acknowledge the enduring pain of some sufferers and instances of “post–Lyme disease syndrome,” there is a great deal of controversy over the use of longer-term courses of antibiotics. Research has shown that Lyme spirochetes can take hold in a patient, even in the face of aggressive antibiotics, making Lyme a “recalcitrant and chronic relapsing infection.” Identifying those patients and how best to treat them remains a challenge, making chronic Lyme a complicated and disputed clinical beast.
The IDSA’s recommendations are particularly controversial given an antitrust investigation undertaken by the attorney general of Connecticut. In 2008, that investigation reported that the IDSA did not perform a conflict-of-interest review for any of the panelists on the recommendation committee, and that several panelists had financial connections to insurance companies and Lyme vaccine manufacturers. Those who acknowledge the existence of chronic Lyme disease were blocked from appointment to the panel.
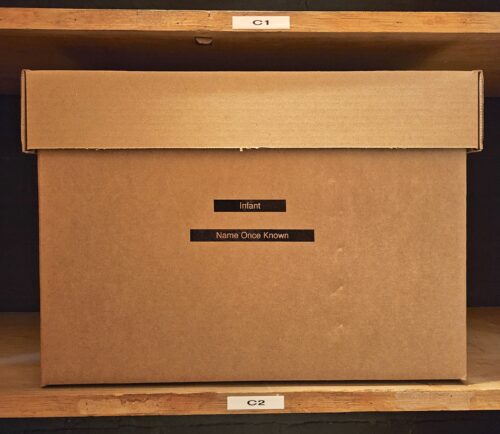
All this leaves many people like myself to fend for ourselves as we suffer the horrors of unrecognized or misunderstood illness. It’s hard to say how many around the world have chronic Lyme disease—but we need to recognize the potentially serious and disabling nature of Lyme and how it has been mismanaged by the U.S. medical system and the government. It’s critical we increase research for better diagnosis and treatment.
After a year and a half, I experienced a brief period of remission. I resumed my regular activities, spent time with my children, and started training again. (I was a kickboxer in my former life.) But the reprieve only lasted a few months. Before long, I was bedridden again by numbness, nerve pain, tremors, and bone-deep exhaustion.
One night, two years into my illness, I experienced heart pains that dropped me to my knees. My partner rushed me to the hospital, and the medical staff decided to keep me overnight. In the morning, the cardiologist dismissed my blood pressure of 144 as “slightly elevated.” He struck me as aloof, even sneering. In my own eyes, I was a boxer with a normal resting heart rate of 55 and a blood pressure of 110—and I had an extreme and unusual set of symptoms that were cause for concern. But to him, I was just a statistical fragment; he saw no reason to give a second thought to my claim that this number was abnormally high for me. While interacting with him, I felt like I had lost an essential part of myself. The “healthy boxer” loomed behind me like a breathing phantom.
Shortly after this clinical encounter, my mental state and behaviors changed. I began spending considerable time picturing what my absence would look like, convincing myself that my loved ones would be better off without me. I didn’t want to end my life. I wanted to escape the terminal collapse of my world.
The sky was pale white with indifference on the morning I tried to kill myself. When I didn’t answer my phone, my partner instinctively felt that there was something wrong. She headed home and called an ambulance. I spent the next weeks in a mental health facility in a state of depressive catatonia. I don’t remember much beyond the green walls, gray carpet, my neighbor’s singing sessions in the shower, and the smell of cigarette smoke. I knew then, as I do now, that I had fallen prey to something darker, more powerful, and much more ancient than myself.
For the rest of my life, I will struggle to incorporate my attempted suicide into my sense of self. Trying to explain the medical, psychological, and sociocultural conditions surrounding it has been one way of working to come to terms with my illness and related experiences.
Suicide and suicidal thoughts are not unusual in the village of the sick. It is estimated that around 44,000 people killed themselves in 2015 in the United States; as many as 1,200 suicides annually might be attributed to Lyme and associated diseases, according to a study that scaled up one doctor’s chart review of more than 250 patients with Lyme.
There are plausible biological explanations for suicide and suicidal thoughts among those with Lyme: Studies have shown strong connections between brain inflammation, immune response, and suicide. But just as important are psychological factors associated with the combination of pain, suffering, and frustration patients experience with inadequate care. In 2015, a 41-year-old man who likely had Lyme for nine years before finally being diagnosed with the disease took his own life. The anxiety and pain he experienced were relentless, his fiance said.
My own experiences with Western medicine confirm what many others have argued: Inadequate care is in part shaped by biased research, power imbalances, and mistaken perceptions. Biological differences between men and women, for example, are known to impact diagnostics and treatment: The disproportionate study of men in clinical trials and other studies has skewed our medical knowledge. For instance, heart attacks are sometimes missed entirely in women because women are less likely than men to experience chest pain as a major symptom.
Inaccurate and gendered assumptions on the part of medical practitioners also impact the degree of autonomy and credibility that individuals are granted when recounting their illness experience. I have often wondered if stress was presumed to be at the helm of my alleged psychological disorder because I am a man—just as women are more often diagnosed with “conversion disorders,” formerly referred to as hysteria, in cases where psychic turmoil is attributed to unexplainable bodily dysfunction.
Those with inexplicable conditions often face a similar bias: a tendency for some doctors to dismiss out of hand individuals who have complex and unusual cases. In cases of controversial illnesses, such as myalgic encephalomyelitis (a.k.a. chronic fatigue syndrome), patients can be belittled as “malingerers,” just as those with Lyme disease are sometimes disrespectfully called “Lyme loonies.” I am not suggesting these practices and behaviors are systematically carried out on purpose or maliciously, but rather that they are based on tacit assumptions that influence the ways medical practitioners act.
The doctors I met often struck me as arrogant and unwilling to really sit and listen, making it easy for the complexities surrounding my illness to be misconstrued or not even conveyed, despite my desire to communicate them. Perhaps these doctors would have blamed me for being a bad oral historian. I grew increasingly nervous and insecure as doctors asserted their patriarchal authority. I developed iatrophobia, a deep dread of doctors. And I started to see myself as someone damaged, with an unreliable testimony. My body, my medium for experiencing the world, was transmogrified during these clinical encounters into something without personal meaning. Doctors overlooked what my illness felt like to me and how I experienced it within the context of my life, foreclosing other possible lines of therapeutic options—and my need for understanding and care.
I wonder what would have happened if I had met doctors early on in my illness who were committed to listening empathetically and to practicing a style of medicine informed by humility, receptivity, and compassion. I don’t believe such an approach requires additional resources or time (although those would help), just an adherence to a different set of social and cultural values.
Critics sometimes claim that doctors who recognize and treat chronic Lyme disease are doing so dishonestly, exploiting others’ suffering for their own gain. Maybe there are some who do. But I believe many of these doctors, who risk sanctions by medical boards for treatment strategies that break conventional protocols, are practicing existential medicine: They acknowledge that patients need not just answers but also understanding and comfort. For them, medical care is not only about easing suffering but about becoming an empathetic witness to suffering.
At the moment, I am in a better place. Hyperthermia treatment at a clinic in Germany helped ease some of my symptoms. But I still struggle with debilitating symptoms from my illness and large debts from the costs of seeking treatment. I have had to shed some of my identities that were shattered by my illness and that once defined who I was. I have been forced to understand myself—and give meaning to the world and to my relationships—in new ways. Writing about my illness has helped with this ongoing process of self-remaking.
Almost three years after my tick bite, I now inhabit a space of hope that is every bit as tenuous as the future it anticipates. I know how fragile life is in the throes of illness and how easily it can be clipped with the shears of domination and misunderstanding.